Last updated: September 26, 2016
Edited by:

Associate Professor,
UW Orthopaedics & Sports Medicine

Associate Professor,
UW Orthopaedics & Sports Medicine
Professor,
UW Orthopaedics & Sports Medicine
Follow our blog
http://shoulderarthritis.blogspot.com/
On which we try to provide the best and most current information on shoulder arthritis.
To read more about Shoulder Arthritis, please visit our online Shoulder Arthritis Book.
Contact
If you have questions regarding this procedure, feel free to email Frederick A. Matsen III, M.D. at matsen@uw.edu.
Not all surgical cases are the same, this is only an example to be used for patient education.
Download this article in pdf format.
Summary
Total shoulder replacement arthroplasty is a well-established surgery for restoring comfort and function to the arthritic shoulder. In this procedure the arthritic ball is replaced by a smooth metal ball fixed to the arm bone (humerus) by a stem that fits within it. The arthritic socket (glenoid) is resurfaced with high-density polyethylene prosthesis. Among the different surgical options this procedure appears to provide the most rapid and complete improvement in comfort and function for shoulders with arthritis. Success requires technical excellence of the surgery and a commitment to the exercise program until the desired range of motion can be achieved comfortably.
What Are The Key Parts Of The Normal Shoulder Joint?
The ball (humeral head) fits in the socket (glenoid) and is held there by the rotator cuff.
What Is Shoulder Arthritis?
Shoulder arthritis is a condition in which degeneration, injury, inflammation or previous surgery destroys the normally smooth cartilage on the ball (humeral head) and socket (glenoid).
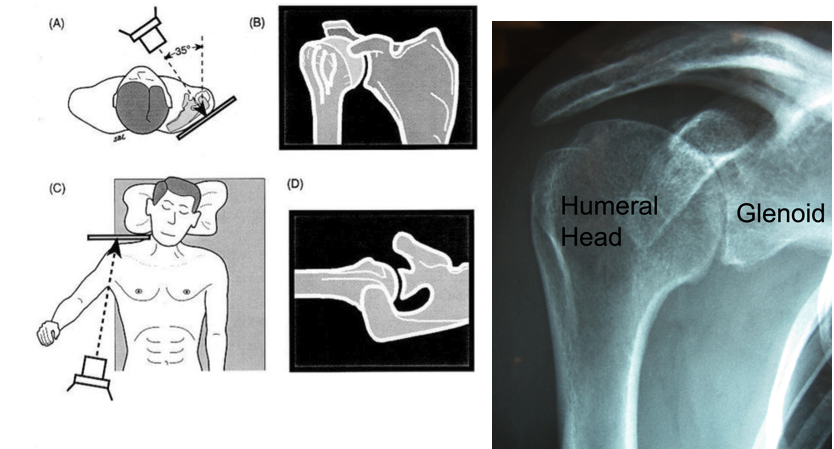
How Is Shoulder Arthritis Diagnosed?
Carefully standardized X-rays reveal the loss of the space between the humeral head and glenoid that is normally occupied by cartilage, leaving bone on bone contact.
What Is A Total Shoulder?
In a total shoulder, the arthritic surface of the ball is replaced with a metal ball with a stem that is press fit in the inside of the arm bone (humerus) and the socket is resurfaced with a high density polyethylene component.
After a general or regional anesthetic, this procedure is performed through an incision between the deltoid and the pectoralis major muscles on the front of the shoulder. It includes release of adhesions and contractures and removal of bone spurs that may block range of motion. Our team of surgeons, anesthesiologists, and surgical assistants usually perform this procedure in less than two hours.
The arthritic surface of the ball is replaced with a metal ball with a stem that is press fit down the inside of the arm bone (humerus) so that only the smooth surface extends from the bone.
How Is The Humeral Component Fixed In The Humerus?
While some surgeons cement the humeral component and others use implants that foster bone ingrowth, we find that these approaches stiffen the bone making it more likely to fracture in a fall on one hand and greatly complicating any revision surgery that may become necessary in the future on the other. We prefer to fix the component by impaction grafting the inside of the humerus (using bone harvested from the humeral head that has been removed) until a tight press fit of the implant is achieved.
How Is The Glenoid Component Fixed To The Glenoid Bone?
The bone of the glenoid is precisely shaped with a glenoid reamer and then the glenoid component is secured with a combination of press fitting and cementing.
In order for proper healing to occur, the patient must maintain the range of motion achieved at surgery with simple, frequent stretching exercises. Rehabilitative exercises are started immediately after surgery using continuous passive motion and stretching by the patient.
Attaining and maintaining at least 150 degrees of forward elevation is critical to the success of this procedure. The forward lean and the supine stretch can be helpful in getting there and maintaining this range of motion.
Who Should Consider A Total Shoulder?
Surgery for shoulder arthritis should only be considered when the arthritis is limiting the quality of the patient’s life and after a trial of physical therapy and mild analgesics. Severe arthritis is usually best managed by either a partial or a complete joint replacement. Total shoulder arthroplasty (replacing the surfaces of both the ball and the socket) is usually considered by individuals who want the best chance of a rapid recovery of shoulder comfort and the ability to perform activities of daily living.
Who Should Probably Not Consider A Total Shoulder Replacement?
This procedure is less likely to be successful in individuals with depression, obesity, diabetes, Parkinson’s disease, multiple previous shoulder surgeries, shoulder joint infections, rotator cuff deficiency and severely altered shoulder anatomy.
What Are The Keys To Success Of A Total Shoulder?
Success requires technical excellence of the surgery and participation by the patient in a simple exercise program until the desired range of motion can be achieved comfortably.
How Does A Patient Prepare For The Total Shoulder Procedure?
As for all elective surgical procedures, the patient should be in the best possible physical and mental health at the time of the procedure. Any heart, lung, kidney, bladder, tooth, or gum problems should be managed before surgery. Any infection may be a reason to delay the operation. Any skin problem (acne, scratches, rashes, blisters, burns, etc) on the shoulder or arm should be resolved before surgery. The shoulder surgeon needs to be aware of all health issues, including allergies as well as the non-prescription and prescription medications being taken. For instance, aspirin and anti-inflammatory medication may affect the way the blood clots. Some of these may need to be modified or stopped before the time of surgery.
What Happens After Surgery?
Total shoulder arthroplasty is a major surgical procedure that involves cutting of skin, tendons and bone. The pain from this surgery is managed by the anesthetic and by pain medications. Immediately after surgery, strong medications (such as morphine or Demerol) are often given by injection. Within a day or so, oral pain medications (such as hydrocodone or Tylenol with codeine) are usually sufficient. The shoulder rehabilitation program is started on the day of surgery. The patient is encouraged to be up and out of bed soon after surgery and to progressively reduce their use of pain medications. Hospital discharge usually takes place on the second or third day after surgery. Patients are to avoid lifting more than one pound, pushing and pulling for six weeks after surgery. Driving is recommended only after the shoulder has regained comfort and the necessary motion and strength. This may take several weeks after surgery. Thus the patient needs to be prepared to have less arm function for the first month or so after surgery than immediately before surgery. For this reason, patients usually require some assistance with self-care, activities of daily living, shopping and driving for approximately six weeks after surgery. Management of these limitations requires advance planning to accomplish the activities of daily living during the period of recovery.
What About Rehabilitation?
Early motion after a total shoulder replacement is critical for achieving optimal shoulder function. Arthritic shoulders are stiff. Although a major goal of the surgery is to relieve this stiffness by release of scar tissue, it may recur during the recovery process if range of motion exercises are not accomplished immediately. For the first 6 weeks of the recovery phase, the focus of rehabilitation is on maintaining the motion that was recovered at surgery. Strengthening exercises are avoided during the first 6 weeks so as not to stress the tendon repair before it heals back to the bone. Later on, once the shoulder is comfortable and flexible, strengthening exercises and additional activities are started. Some patients prefer to carry out the rehabilitation program themselves. Others prefer to work with a physical therapist who understands the total shoulder program.
When Can Ordinary Daily Activities Be Resumed?
In general, patients are able to perform gentle activities of daily living using the operated arm from two to six weeks after surgery. Walking is strongly encouraged. Driving should wait until the patient can perform the necessary functions comfortably and confidently. Recovery of driving ability may take six weeks if the surgery has been performed on the right shoulder, because of the increased demands on the right shoulder for shifting gears. With the consent of their surgeon, patients can often return to activities such as swimming and golf at six months after their surgery.
Click to enlarge
An incision between
the deltoid and
the pectoralis major muscles
on the front of the shoulder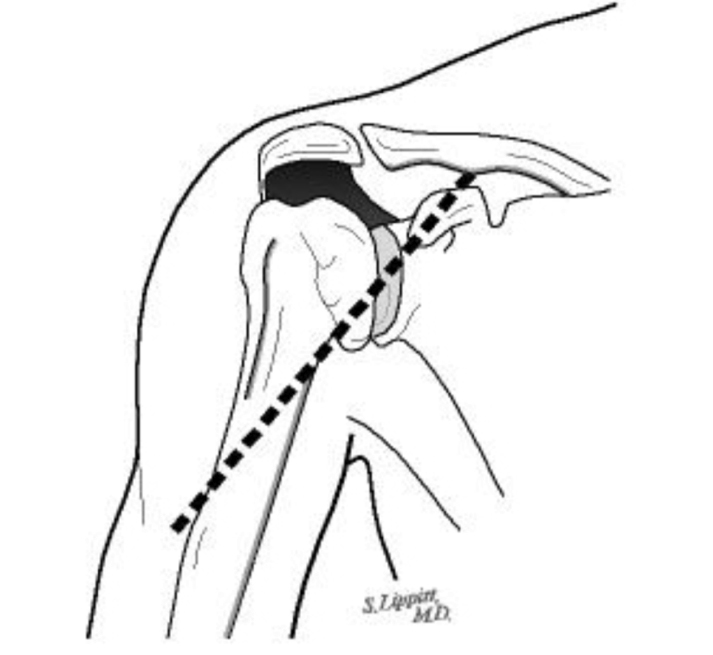
Click to enlarge
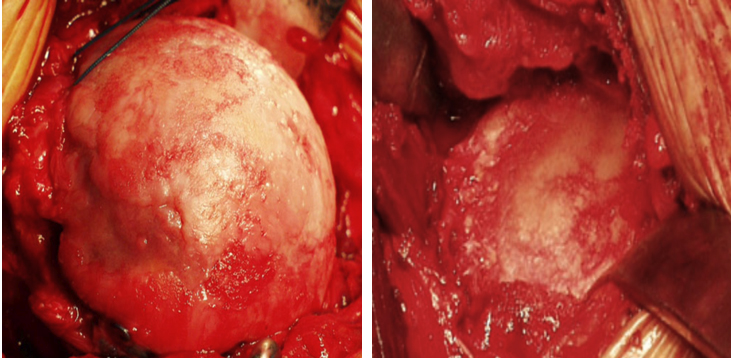
The arthritic surface
of the ball is replaced
with a metal ball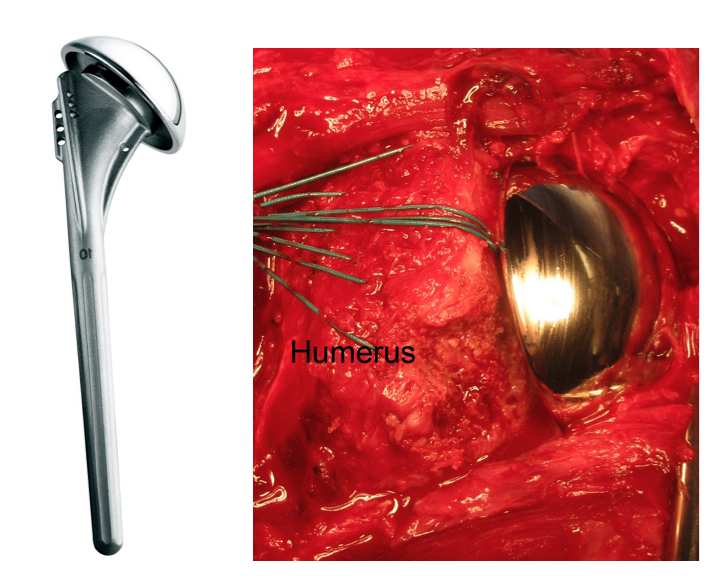
Click to enlarge
The Glenoid Component
Fixed To The Glenoid Bone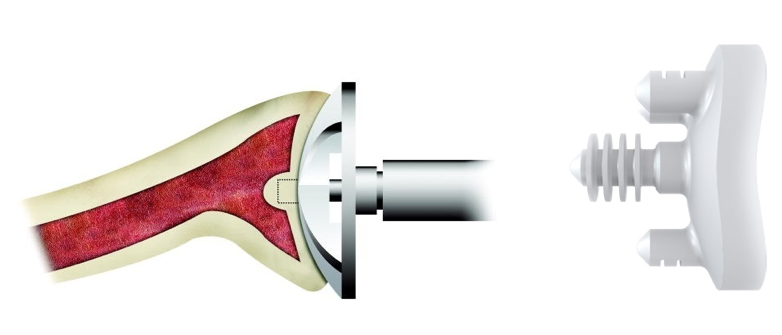
Click to enlarge
Rehabilitative exercises are
started immediately after surgery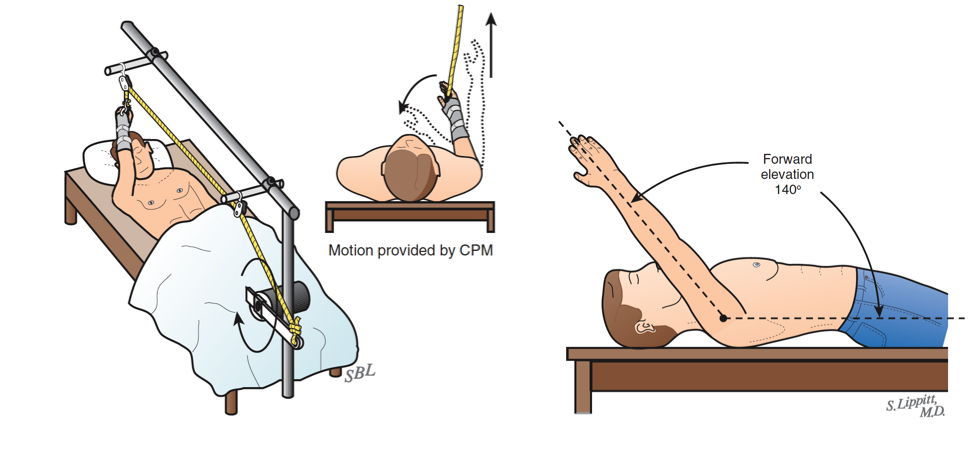
Click to enlarge
Attaining and maintaining
at least 150 degrees
of forward elevation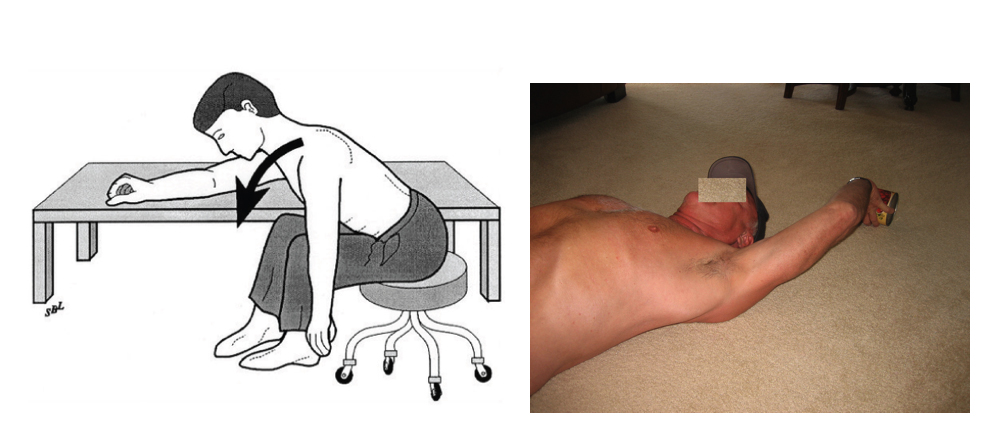
Once A Shoulder With A Total Shoulder Procedure Has Successfully Completed The Rehabilitation Program, What Activities Are Permissible?
Once the shoulder has a nearly full range of motion, strength and comfort, we recommend that the shoulder be protected from heavy lifting loads and from impact. Thus we discourage chopping wood, training with heavy weights, vigorous hammering, and recreational activities that subject the shoulder to impact loading.
What Problems Can Complicate A Total Shoulder And How Can They Be Avoided?
Like all surgeries, the total shoulder operation can be complicated by infection, nerve or blood vessel injury, fracture, instability, component loosening, and anesthetic complications. Furthermore, this is a technically exacting procedure and requires an experienced surgeon to optimize the bony, prosthetic and soft tissue anatomy after the procedure. The procedure can fail if the reconstruction is too tight, too loose, improperly aligned, insecurely fixed or if unwanted bone-to-bone contact occurs. The most common cause of failure in the short term is a patient’s inability to maintain the range of motion achieved at surgery during the healing period, which can last up to six months after surgery. The most common long-term problem is wearing or loosening of the glenoid component.
How Many Total Shoulder Surgeries Are Done At The University Of Washington?
We currently perform over 80 of these procedures per year.
What If The Patient Lives A Long Way Away From Seattle?
Patients often come to Seattle from a long distance for the procedure. We are available by appointment in the Shoulder and Elbow Clinic, 4245 Roosevelt Way N.E. Seattle, on Mondays and Fridays to evaluate individuals with shoulder arthritis to discuss the procedures that might be most ideally suited for them. We perform surgery on Tuesdays and Wednesdays at the University of Washington Medical Center, 1959 NE Pacific St, Seattle, Washington, 206 598-4288. We also see patients at the Eastside Specialty Center, 1700 - 116th Ave NE, Bellevue, Washington, 425 646-7777. Patients having a total shoulder are usually able to return home three days after the procedure, assuming they have mastered their exercises. The staples used to close the skin can be removed by a nurse or physician near the patient’s home. Ideally, we like to see patients back at six weeks after surgery to assure that satisfactory progress is being made. We request that patients complete questionnaires at 3, 6, 12, 18 and 24 months after surgery so we can track their progress and that the patient obtain and send to us X-rays at 12 and 24 months after surgery if they are unable to return to Seattle for the annual follow-ups. All patients have our personal email and the clinic contact phone numbers to use in contacting us at any time questions arise.
Conclusion
Summary Of The Total Shoulder Procedure For Arthritis Of The Shoulder Total shoulder arthroplasty is a well-established procedure for restoring comfort and function to shoulders damaged by arthritis. In the hands of an experienced surgeon, total shoulder replacement can be an effective method for treating shoulders with damaged joint surfaces in a healthy and motivated patient. Pre-planning and persistent rehabilitation efforts will help assure the best possible result for the patient.
Frederick A. Matsen III and Winston J. Warme
Shoulder Surgeons
University of Washington
Department of Orthopaedics and Sports Medicine
References:
Matsen III, F.A.: Early Effectiveness of Shoulder Arthroplasty for Patients Who Have Primary Glenohumeral Degenerative Joint Disease. J. Bone and Joint Surgery, 78-A(2):260-264, 1996.
Matsen III, F.A., Smith, K.L., DeBartolo, S.E., and Von Oesen, G.: A comparison of patients with late-stage rheumatoid arthritis and osteoarthritis of the shoulder using self-assessed shoulder function and health status. Arthritis Care and Research 10:43-47, 1997.
Rozencwaig, R., van Noort, A., Moskal, M.J., Smith, K.L., Sidles, J.A., and Matsen III, F.A.: The Correlation of Comorbidity with Shoulder Function and Health Status in Patients with Glenohumeral Degenerative Joint Disease. J. Bone and Joint Surg., 80-A(8):1146-1153, 1998.
Matsen, F.A., III, Antoniou, J., Rozencwaig, R., Campbell, B., and Smith, K.L.: Correlates with comfort and function after total shoulder arthroplasty for degenerative joint disease. J. Shoulder Elbow Surg., 9(6):465-469, 2000. Goldberg, B.A., Smith, K.L., Jackins, S., Campbell, B., and Matsen III, F.A.: The magnitude and durability of functional improvement after total shoulder arthroplasty for degenerative joint disease. J. Shoulder Elbow Surg., 10(5):464-469, 2001.
Boorman, R., Hacker, S., Lippitt, S.B., and Matsen III, F.A.: A Conservative Broaching and Impaction Grafting Technique for Humeral Component Placement and Fixation in Shoulder Arthroplasty: The Procrustean Method. Techniques in Shoulder & Elbow Surgery. 2(3): 166-175, September 2001.
Fehringer, E.V., Kopjar, B., Boorman, R.S., Churchill, R.S., Smith, K.L., and Matsen III, F.A.: Characterizing the functional improvement after total shoulder arthroplasty for osteoarthritis. J. Bone Joint Surg., 84A(8):1349-1353, 2002.
Hasan, S.S., Leith, J.M., Campbell, B., Kapil, R., Smith, K.L., and Matsen III, F.A.: Characteristics of unsatisfactory shoulder arthroplasties. J. Shoulder Elbow Surg., 11(5):431-441, 2002.
Lazarus, M.D., Jensen, K.L., Southworth, C., and Matsen III, F.A.: The radiographic evaluation of keeled and pegged glenoid component insertion. J. Bone Joint Surg., 84A(7):1174-1182, 2002.
Matsen III, F.A.: The relationship of surgical volume to quality of care: scientific considerations and policy implications. J. Bone Joint Surg., 84A(8):1482-1483, discussion 1483-1485, 2002.
Hacker, S., Boorman, R., Lippitt, S.B., and Matsen III, F.A.: Impaction grafting improves the fit of proximal humeral arthroplasty. JSES, 12(5):431-435, 2003.
Boorman, R., Kopjar, B., Fehringer, E., Churchill, R.S., Smith, K.L., and Matsen III, F.A.: The effect of total shoulder arthroplasty on self-assessed health status is comparable to that of total hip arthroplasty and coronary artery bypass grafting. J. Shoulder Elbow Surg., 12(2): 158-163, 2003.
Hasan, S., Leith, J., Smith, K.L., and Matsen III, F.A.: The distribution of shoulder replacements among surgeons and hospitals is significantly different than that of hip or knee replacements. J. Shoulder and Elbow Surg., 12(2): 164-169, 2003.
Matsen III, F.A., Rockwood Jr., C.A., and Iannotti, J.: Humeral fixation by press fit of a tapered metaphyseal stem. A prospective radiograph study. J. Bone Joint Surg., 85A(2): 304-308, 2003.
Parsons, I.M. 4th, Campbell, B., Titelman, R.M., Smith, K.L., Matsen, F.A. III: Characterizing the effect of diagnosis on presenting deficits and outcomes after total shoulder arthroplasty. J Shoulder and Elbow Surg 14 (6): 575-94, 2005.
Churchill, R., Kopjar, B., Fehringer, E., Boorman, R., Matsen, F.A. III: Humeral Component Modularity May Not Be an Important Factor in the Outcome of Shoulder Arthroplasty for Glenohumeral Osteoarthritis. Am J Orthop 34 (4): 173-176, 2005.
Franta AK, Lenters TR, Mounce D, Neradilek B, Matsen FA 3rd. The complex characteristics of 282 unsatisfactory shoulder arthroplasties. J Shoulder Elbow Surg. 2007 Sep-Oct;16(5):555-62.
Matsen FA 3rd, Bicknell RT, Lippitt SB. Shoulder arthroplasty: the socket perspective. J Shoulder Elbow Surg. 2007 Sep-Oct;16(5 Suppl):S241-7.
Lee M, Chebli C, Mounce D, Bertelsen A, Richardson M, Matsen F 3rd.Intramedullary reaming for press-fit fixation of a humeral component removes cortical bone asymmetrically. J Shoulder Elbow Surg. 2008 Jan-Feb;17(1):150-5.
Matsen FA 3rd, Clinton J, Lynch J, Bertelsen A, Richardson ML. Glenoid Component Failure in Total Shoulder Arthroplasty. J Bone Joint Surg, 2008 Apr;90(4):885-96.
127