Last Updated: November 16, 2007
After an initial dislocation the shoulder may return to functional stability or it may fall victim to recurrent glenohumeral instability. While intermediate forms of recurrent instability do occur the great majority of recurrently unstable shoulder may be thought of as being either atraumatic or traumatic in origin.
JBJS Article on Shoulder Dislocation (PDF) (2.66 MB)
Atraumatic instability is instability that arises without the type of trauma necessary to tear the stabilizing soft tissues or to create a humeral head defect tuberosity fracture or glenoid lip fracture.
AMBRII syndrome
Certain shoulders may be more susceptible to atraumatic instability. A small or functionally flat glenoid fossa may jeopardize the concavity compression adhesion-cohesion and glenoid suction cup stability mechanisms. Thin excessively compliant capsular tissue may invaginate into the joint when traction is applied limiting the effectiveness of stabilization from limited joint volume. A large potentially capacious capsule may allow humeroscapular positions outside the range of balance stability.
Weak rotator cuff muscles may provide insufficient compression for the concavity compression stabilizing mechanism. Poor neuromuscular control may fail to position the scapula to balance the net humeral joint reaction force. Voluntary or inadvertent malpositioning of the humerus in excessive anterior or posterior scapular planes may cause the net humeral joint reaction force to lie outside balance stability angles. Once initiated the instability may be perpetuated by compression of the glenoid rim resulting from chronically poor humeral head centering. Excessive labral compliance may predispose to this loss of effective glenoid depth.
Any of these factors individually or in combination could contribute to instability of the glenohumeral joint. For example posterior glenohumeral subluxation may result from the combination of a relatively flat posterior glenoid and the tendency to retract the scapula during anterior elevation of the arm resulting in use of the elevated humerus in excessively anterior scapular planes. Excessively compliant capsular tissue in combination with relatively weak rotator cuff muscles could contribute to inferior subluxation on attempted lifting of objects with the arm at the side. If the lateral scapula is allowed to droop (whether voluntarily or involuntarily) the superior capsular structures are relaxed permitting inferior translation of the humerus with respect to the glenoid (see figure 1). (Itoi et al 1993)
Because they usually result from loss of midrange stability atraumatic instabilities are more likely to be multidirectional. Pathogenic factors such as a flat glenoid weak muscles and a compliant capsule may produce instability anteriorly inferiorly posteriorly or a combination. Although the onset of atraumatic instability may be provoked by a period of disuse or a minor injury many of the underlying contributing factors may be developmental. As a result the tendency for atraumatic instability is likely to be bilateral and familial as well.
It is apparent that atraumatic instability is not a simple diagnosis but rather a syndrome that may arise from a multiplicity of factors. To help recall the various aspects of this syndrome we use the acronym AMBRII. The instability is Atraumatic usually associated with Multidirectional laxity and with Bilateral findings. Treatment is predominantly by Rehabilitation directed at restoring optimal neuromuscular control. If surgery is necessary it needs to include reconstruction of the rotator Interval capsule-coracohumeral ligament mechanism and tightening of the Inferior capsule. The diagnosis and management of this condition has been presented in detail. (Cofield 1993; Lippitt et al 1991; Matsen Lippitt Sidles et al 1994; O'Driscoll 1993)
AMBRII history
Most patients presenting with AMBRII are under the age of 30 years (see figure 2). Because the instability manifests itself in mid range positions of the shoulder atraumatic instability typically causes discomfort and dysfunction in ordinary activities of daily living. Commonly such patients have greatest difficulty sleeping lifting overhead and throwing (see table 1 and figure 3). Their general health status as revealed by the SF 36 is not as good on average as that of a comparable group of patients with traumatic instability (see figure 4).
Table 1
| TUBS | AMBRII | Failed Repairs | |
| Number of Patients | 101 | 70 | 76 |
| % female | 26% | 38% | 28% |
| % right side | 55% | 68% | 51% |
| Age | 29±11 | 27±10 | 31 ± 8 |
| % able to perform SST function | TUBS (101) | AMBRII (70) | Failed Repairs (76) |
| Sleep on Side | 43 | 19 | 11 |
| Place 1 lb on shelf | 91 | 75 | 65 |
The onset is usually insidious but it may occur after a minor injury or period of disuse. The unwanted translations may range from a sensation of a minor "slip" in the joint to a complete dislocation of the humeral head from the glenoid. The displacement characteristically reduces spontaneously after which the patient is usually able to return to his or her activities without much pain or problem. As the condition progresses the patient notices that the shoulder has become looser and may feel it slip out and clunk back in with increasing ease and in an increasing number of activities. The shoulder may become uncomfortable even with the arm at rest. The patient may volunteer that he or she can make the shoulder "pop out" and that at times the shoulder feels as if it "needs to be popped out" on purpose.
It is important to document from the history the circumstances surrounding the onset of the problem as well as each and every position of the shoulder in which the patient experiences instability. It is also important to note if the opposite shoulder is symptomatic as well.
A family history may reveal other kindred similarly affected as well as conditions know to predispose to atraumatic instability such as Ehlers Danlos syndrome.
Many patients admit that they used to have a habit of dislocating the joint but now they can no longer control the stability of the joint. The surgeon must determine if habitual dislocation remains a feature of the patients problem. It is obvious that it is difficult for surgery to cure habitual instability.
Finally it is important to document the patient's expectations of their shoulder to assure that the goals are within reach before treatment is started.
Demonstration of instability
The patient is routinely asked if he or she can dislocate the shoulder at will. This enables the surgeon to see the different positions of concern and directions of translation. By palpating the scapula the surgeon can estimate the relative position of the humerus and scapula when the shoulder is translated and reduced. There are three common demonstrations of instability:
- The patient may demonstrate a spontaneous "jerk" test by bringing the internally rotated arm horizontally across the chest causing the humeral head to subluxate posteriorly. Then by returning the elevated humerus to the coronal plane the shoulder produces a "clunk" on reduction of glenohumeral joint (much like the Ortolani and Barlow signs of the hip).
- The patient may demonstrate that when he or she attempts to lift an object or tie a shoe the shoulder subluxates inferiorly.
- The patient may demonstrate that the shoulder translates when the arm is elevated in posterior humerothoracic planes with spontaneous reduction on return to the coronal plane.
Laxity tests
These tests examine the amount of translation allowed by the shoulder starting from positions where the ligaments are normally loose. The amount of translation on laxity testing is determined by the length of the capsule and ligaments as well as by the starting position (i.e. more anterior laxity will be noted if the arm is examined in internal rotation--which relaxes the anterior structures than if it is examined in external rotation--which tightens the anterior structures).
In interpreting the significance of the degree of translation on laxity tests it is important to use the contralateral shoulder as an example of what is "normal" for the patient. Not infrequently the laxity on the symptomatic side will be similar to that on the asymptomatic side. Investigations of clinical laxity tests showed that the range of translations for shoulders with atraumatic instability was similar to that of normal shoulders or shoulders with traumatic instability (see figure 5). (Harryman Sidles and Matsen 1992) However a distinguishing feature of many shoulders with atraumatic instability is that the resistance to translation is diminished when the humeral head is pressed into the glenoid fossa; suggesting that the effective glenoid concavity is diminished. It is helpful if the patient recognizes one or more of the directions of translation as being responsible for his or her clinical symptoms. Finally it is important to point out that these are tests of laxity not tests for instability: Many normally stable shoulders such as those of gymnasts will demonstrate substantial translation on these laxity tests even though they are asymptomatic.
Drawer test
The patient is seated with the forearm resting on the lap and the shoulder relaxed. The examiner stands behind the patient. One of the examiner's hands stabilizes the shoulder girdle (scapula and clavicle) while the other grasps the proximal humerus. These tests are performed with (1) a minimal compressive load (just enough to center the head in the glenoid) and (2) with a substantial compressive load (to gain a feeling for the effectiveness of the glenoid concavity). Starting from the centered position with a minimal compressive load the humerus is first pushed forward to determine the amount of anterior displacement relative to the scapula. The anterior translation of a normal shoulder reaches a firm end-point with no clunking no pain and no apprehension. A clunk or snap on anterior subluxation or reduction may suggest a labral tear or Bankart lesion. The test is then repeated with a substantial compressive load applied before translation is attempted to gain an appreciation of the competency of the anterior glenoid lip. The humerus is returned to the neutral position and the posterior drawer test is performed with light and again with substantial compressive loads to judge the amount of translation and the effectiveness of the posterior glenoid lip respectively. (Silliman and Hawkins 1993)
Sulcus test
The patient sits with the arm relaxed at the side. The examiner centers the head with a mild compressive load and then pulls the arm downward. Inferior laxity is demonstrated if a sulcus or hollow appears inferior to the acromion. Competency of the inferior glenoid lip is demonstrated by pressing the humeral head into the glenoid while inferior traction is applied.
Push-pull test
The patient lies supine with the shoulder off the edge of the table. The arm is in 90 degrees of abduction and 30 degrees of flexion. Standing next to the patient's hip the examiner pulls up on the wrist with one hand while pushing down on the proximal humerus with the other. The shoulders of normal relaxed patients often will allow 50 per cent posterior translation on this test.
Stability tests
These tests examine the ability of the shoulder to resist challenges to stability in positions where the ligaments are normally under tension.
Fulcrum test
The patient lies supine at the edge of the examination table with the arm abducted to 90 degrees. The examiner places one hand on the table under the glenohumeral joint to act as a fulcrum. The arm is gently and progressively extended and externally rotated over this fulcrum. Maintaining gentle passive external rotation for a minute fatigues the subscapularis challenging the capsular contribution to the anterior stability of the shoulder. The patient with anterior instability will usually become apprehensive as this maneuver is carried out (watch the eyebrows for a clue that the shoulder is getting ready to dislocate). In this test normally no translation occurs because it is performed in a position where the anterior ligaments are placed under tension.
Crank or apprehension test
The patient sits with the back toward the examiner. The arm is held in 90 degrees of abduction and external rotation. The examiner pulls back on the patient's wrist with one hand while stabilizing the back of the shoulder with the other. The patient with anterior instability usually will become apprehensive with this maneuver. As for the fulcrum test no translation is expected in the normal shoulder because this test is performed in a position where the anterior ligaments are placed under tension.
Jerk test
The patient sits with the arm internally rotated and flexed forward to 90 degrees. The examiner grasps the elbow and axially loads the humerus in a proximal direction. While axial loading of the humerus is maintained the arm is moved horizontally across the body. A positive test is indicated by a sudden jerk as the humeral head slides off the back of the glenoid. When the arm is returned to the original position of 90-degree abduction a second jerk may be observed that of the humeral head returning to the glenoid.
Strength tests
The strength of abduction and rotation are tested to gauge the power of the muscles contributing to stability through concavity compression. The strength of the scapular protractors and elevators are also tested to determine their ability to position the scapula securely.
Radiographs
In atraumatic instability shoulder radiographs characteristically show no bony pathology. Specifically there is no posterolateral humeral head defect no glenoid rim fracture or new bone formation and no evidence of tuberosity fracture. Because these patients characteristically demonstrate midrange instability radiographs may show translation of the humeral head with respect to the glenoid; for example the axillary view may show posterior subluxation. Occasionally radiographs may suggest factors underlying the atraumatic instability such as a relatively small or hypoplastic glenoid or a posteriorly inclined or otherwise dysplastic glenoid. The bony glenoid fossa may appear quite flat; however it is difficult to relate the apparent depth of the bony socket to the effective depth of the fossa formed by cartilage and labrum covering the bone.
We do not use stress radiographs arthrography MRI or arthroscopy in the diagnosis of atraumatic instability.
Traumatic instability is instability that arises from an injury of sufficient magnitude to tear the glenohumeral capsule ligaments labrum or rotator cuff or to produce a fracture of the humerus or glenoid.
TUBS
A typical patient is a 17-year-old skier whose recurrent anterior instability began with a fall on an abducted externally rotated arm (although the condition has been reported in individuals as young as three years old. (Endo et al 1993) In order to injure these strong structures a substantial force must be applied to them. The most common pathology associated with traumatic instability is the avulsion of the anteroinferior capsule and ligaments from the glenoid rim. Substantial force is required to produce this avulsion in a healthy shoulder. While this load may be applied directly (for example by having the proximal humerus hit from behind) an indirect loading mechanism is more common. Indirect loading is most easily understood in terms of a simple model of the torques involved. When the upper extremity is abducted and externally rotated by a force applied to the hand the following equation for torque equilibrium is a useful approximation if we attribute the major stabilizing role to the ligament (see figure 6): T = B * E/R where "T" is the tension in the inferior glenohumeral ligament "R" is the radius of the humeral head "B" is the abduction external rotation load applied to the hand and "E" is the distance from the center of the humeral head to the hand. If the radius of the humeral head is 2.5 cm and the distance from the head center to the hand is one meter this formula suggests that the inferior glenohumeral ligament would experience a load 40 times greater than that applied to the hand. From this example we can see that a relatively small load is required to produce the characteristic lesion of traumatic instability if this load is applied indirectly through the lever arm of the upper extremity.
Avulsion of the anterior glenohumeral ligament mechanism (see figure 7) deprives the joint of stability in positions where this structure is a check rein such a in maximal external rotation and extension of the arm elevated near the coronal plane. Thus it is evident that in recurrent traumatic instability problems are most likely to occur when the arm is placed in a position approximating that in which the original injury occurred. Midrange instability may also result from a traumatic injury because the glenoid concavity may be compromised by avulsion of the labrum or fracture of the bony lip of the glenoid (see figure 8). Lessening of the effective glenoid arc compromises the effectiveness of concavity compression reduces the balance stability angles reduces thesurface available for adhesion-cohesion and compromises the ability of the glenoid suction cup to conform to the head of the humerus.
The corner of the glenoid abuts against the insertion of the cuff to the tuberosity when the humerus is extended abducted and externally rotated (see figure 9). (Liu and Boynton 1993; Matsen Lippitt Sidles et al 1994; Montgomery and Jobe 1994; Rossi et al 1994; Walch et al 1991; Walch et al 1993) Thus the same forces which challenge the inferior glenohumeral ligament are also applied to the greater tuberosity-cuff insertion area. It is not surprising therefore that posterolateral humeral head defects tuberosity fractures and cuff injuries may be a part of the clinical picture of traumatic instability. The exact location and type of traumatic injury depends on the age of the patient and the magnitude rate and direction of force applied. Avulsions of the glenoid labrum glenoid rim fractures and posterolateral humeral head defects are more commonly seen in young individuals. In patients over the age of 35 traumatic instability tends to be associated with fractures of the greater tuberosity and rotator cuff tears. This tendency increases with increasing age at the time of the initial traumatic dislocation. Thus as a rule younger patients require management of anterior lesions and older patients require management of posterior lesions.
The posterior lateral humeral head defect is a common feature of traumatic instability. These lesions are often noted after the first traumatic dislocation and tend to increase in size with recurrent episodes. This impaction injury usually occurs when the anterior corner of the glenoid is driven into the posterior lateral humeral articular surface. It is evident that this injury is close to the cuff insertion. Large head defects compromise stability by diminishing the articular congruity of the humerus.
To help recall the common aspects of traumatic instability we use the acronym TUBS. The instability arises from a significant episode of Trauma characteristically from abduction and extension of the arm elevated in the coronal plane. The resulting instability is usually Unidirectional in the anteroinferior direction.
The pathology is usually an avulsion of the labrum and capsuloligamentous complex from the anterior inferior lip of the glenoid commonly referred to as a Bankart lesion. With functionally significant recurrent traumatic instability a Surgical reconstruction of this labral and ligament avulsion is frequently required to restore stability.
The reader is referred to an review of the pathology and pathogenesis of traumatic instability by Wirth and Rockwood. (Wirth and Rockwood 1993)
TUBS history
Most patients presenting with TUBS are between the ages of 14 and 34 (see figure 10). These patients characteristically have difficulty throwing overhand but many patients also have problems sleeping putting their hand behind their head and lifting a gallon to head level (See table 1 and figure 11). Their general health status as revealed by the SF 36 self assessment questionnaire is better on average than that of a comparable group of patients with atraumatic instability (see figure 12).
Table 1
| TUBS | AMBRII | Failed Repairs | |
| Number of Patients | 101 | 70 | 76 |
| % female | 26% | 38% | 28% |
| % right side | 55% | 68% | 51% |
| Age | 29±11 | 27±10 | 31 ± 8 |
| % able to perform SST function | TUBS (101) | AMBRII (70) | Failed Repairs (76) |
| Sleep on Side | 43 | 19 | 11 |
| Comfort by side | 87 | 71 | 56 |
| Wash opposite shoulder | 69 | 64 | 39 |
| Hand Behind Head | 77 | 75 | 48 |
| Tuck in Shirt | 89 | 81 | 54 |
| Place 8 lbs on shelf | 53 | 35 | 28 |
| Place 1 lb on shelf | 91 | 75 | 65 |
| Place coin on shelf | 93 | 77 | 73 |
| Toss overhand | 31 | 35 | 15 |
| Do usual work | 69 | 46 | 42 |
The initial dislocation
The most important element in the history is the definition of the original injury. As is evident to anyone who has attempted to recreate these lesions in a cadaver substantial force is required to produce a traumatic dislocation--in most cadaver specimens it is impossible to duplicate the Bankart injury mechanism because the humerus fractures first! In characteristic anterior traumatic instability the structure that is avulsed is the strongest part of the shoulder's capsular mechanism: the anterior inferior glenohumeral ligament. In order to tear this ligament substantial force needs to be applied to the shoulder when the arm is in a position to tighten this ligament. Thus the usual mechanism of injury involves the application of a large extension-external rotation force to the arm elevated near the coronal plane. Such a mechanism may occur in a fall while snow skiing while executing a high speed cut in water skiing in an arm tackle during football with a block of a volleyball or basketball shot or in relatively violent industrial accidents in which a posteriorly directed force is applied to the hand while the arm is abducted and externally rotated. Awkward lifting on the job and rear-end automobile accidents would not be expected to provide the conditions or mechanism for this injury. Direct questioning and persistence are often necessary to elicit a full description of the mechanism of the initial injury including the position of the shoulder and the direction and magnitude of the applied force. Yet this information is critical to establishing the diagnosis.
An initial traumatic dislocation often requires assistance in reduction rather than reducing spontaneously as is usually the case in atraumatic instability. Radiographs from previous emergency room visits may be available to show the shoulder in its dislocated position. Axillary or other neuropathy may have accompanied the glenohumeral dislocation. Any of these findings individually or in combination support the diagnosis of traumatic as opposed to atraumatic instability.
Traumatic instability may occur without a complete dislocation. In this situation the injury produces a traumatic lesion but this lesion is insufficient to allow the humeral head to completely escape from the glenoid. The shoulder may be unstable because as a result of the injury it manifests apprehension or subluxation when the arm is placed near the position of injury. In these cases there is no history of the need for reduction nor radiographs with the shoulder in the dislocated position. Thus the diagnosis rests to an even greater extent on a careful history that focuses on the position and forces involved in the initial episode.
The initial dislocation
The most important element in the history is the definition of the original injury. As is evident to anyone who has attempted to recreate these lesions in a cadaver substantial force is required to produce a traumatic dislocation--in most cadaver specimens it is impossible to duplicate the Bankart injury mechanism because the humerus fractures first! In characteristic anterior traumatic instability the structure that is avulsed is the strongest part of the shoulder's capsular mechanism: the anterior inferior glenohumeral ligament. In order to tear this ligament substantial force needs to be applied to the shoulder when the arm is in a position to tighten this ligament. Thus the usual mechanism of injury involves the application of a large extension-external rotation force to the arm elevated near the coronal plane. Such a mechanism may occur in a fall while snow skiing while executing a high speed cut in water skiing in an arm tackle during football with a block of a volleyball or basketball shot or in relatively violent industrial accidents in which a posteriorly directed force is applied to the hand while the arm is abducted and externally rotated. Awkward lifting on the job and rear-end automobile accidents would not be expected to provide the conditions or mechanism for this injury. Direct questioning and persistence are often necessary to elicit a full description of the mechanism of the initial injury including the position of the shoulder and the direction and magnitude of the applied force. Yet this information is critical to establishing the diagnosis.
An initial traumatic dislocation often requires assistance in reduction rather than reducing spontaneously as is usually the case in atraumatic instability. Radiographs from previous emergency room visits may be available to show the shoulder in its dislocated position. Axillary or other neuropathy may have accompanied the glenohumeral dislocation. Any of these findings individually or in combination support the diagnosis of traumatic as opposed to atraumatic instability.
Traumatic instability may occur without a complete dislocation. In this situation the injury produces a traumatic lesion but this lesion is insufficient to allow the humeral head to completely escape from the glenoid. The shoulder may be unstable because as a result of the injury it manifests apprehension or subluxation when the arm is placed near the position of injury. In these cases there is no history of the need for reduction nor radiographs with the shoulder in the dislocated position. Thus the diagnosis rests to an even greater extent on a careful history that focuses on the position and forces involved in the initial episode.
Subsequent episodes of instability
Characteristically the shoulder with traumatic instability is comfortable when troublesome positions are avoided. However the apprehension or fear of instability may prevent the individual from work or sport. Recurrent subluxation or dislocation may occur when the shoulder is forced unexpectedly into the abducted externally rotated position or during sleep when the patient's active guard is less effective. There may be a history of increasing ease of dislocation as the remaining stabilizing factors are progressively compromised.
The goal of the physical examination is largely to confirm the impression obtained from the history: that a certain combination of arm position and force application produces the actual or threatened glenohumeral instability that is of functional concern to the patient.
Signs and symptoms
If the diagnosis has been rigorously established from the history for example by documented recurrent anterior dislocations it is not necessary to risk redislocation on the physical examination. If such rigorous documentation is not available however the examiner must challenge the ligamentous stability of the shoulder in the suspected position of vulnerability being prepared to reduce the shoulder should a dislocation result.
The most common direction of recurrent traumatic instability is anteroinferior. Stability in this position is challenged by externally rotating and extending the arm elevated to various degrees in the coronal plane. It may be necessary to hold the arm in the challenging position for 1 to 2 minutes to fatigue the stabilizing musculature. When the muscle stabilizers tire the capsuloligamentous mechanism is all that is holding the humeral head in the glenoid. At this moment the patient with traumatic anterior instability becomes apprehensive recognizing that the shoulder is about to come out of joint. This recognition is strongly supportive of the diagnosis of traumatic anterior instability.
The magnitude of translation on the standard tests of glenohumeral laxity does not necessarily distinguish stable from unstable shoulders (see figure 13). However the experienced examiner may detect a diminished resistance to anterior translation on the drawer test when the humeral head is compressed into the glenoid fossa indicating loss of the anterior glenoid lip. This maneuver may also elicit grinding as the humeral head slides over the bony edge of the glenoid from which the labrum has been avulsed or catching as the head passes over a torn glenoid labrum.
Pain on abduction external rotation and extension is not specific for instability. Such pain may relate to shoulder stiffness or alternatively to abutment of the glenoid against the cuff insertion to the head posteriorly. (Matsen Lippitt Sidles et al 1994; Rossi Ternamian Cerciello et al 1994; Walch Liotard Boileau et al 1991; Walch Liotard Boileau et al 1993) Relief of this pain by anterior pressure on the humeral head may result from diminished stretch on the anterior capsule or from relief of the abutment posteriorly (see figure 14).
In all patients with traumatic instability but particularly in those over age 35 the strength of the internal and external rotation must be examined to explore the possibility of cuff weakness or tear. Finally a neurological examination is performed to determine the integrity of the axillary nerve and other branches of the brachial plexus.
Radiographs and other tests
Radiographs frequently help to provide confirmation of traumatic glenohumeral instability.
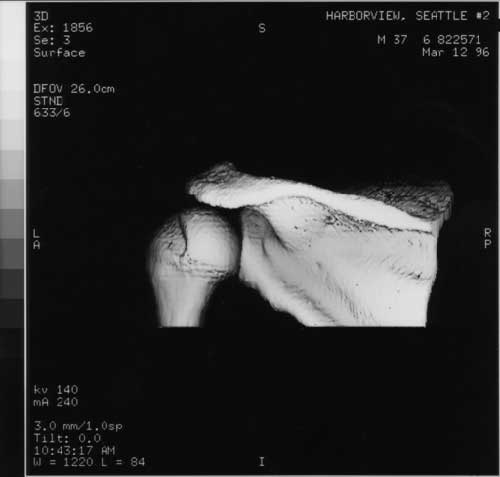
Humeral head changes
One of the most common findings is indentation or impaction in the posterior aspect of the humeral head from contact with the anteroinferior corner of the glenoid when the joint was dislocated (see figures 15 and 16). In their classic article (Hill and Sachs 1940) Hill and Sachs evaluated the relationship of humeral head defects to shoulder instability. They concluded that more than two-thirds of anterior shoulder dislocations are complicated by a bony injury of the humerus or scapula. We quote:
"Compression fractures as a result of impingement of the weakest portion of the humeral head that is the posterior lateral aspect of the articular surface against the anterior rim of the glenoid fossa are found so frequently in cases of habitual dislocation that they have been described as a typical defect. These defects are sustained at the time of the original dislocation. A special sign is the sharp vertical dense medial border of the groove known as the line of condensation the length of which is correlated with the size of the defect."
They reported the defect in only 27 per cent of 119 acute anterior dislocations and in 74 per cent of 15 recurrent anterior dislocations. However they stated that the incidence of the groove defect was low undoubtedly because it was only in the last 6 months of their 10-year study (1930 to 1940) that they used special radiographic views. The size of the defect varied in length (cephalocaudal) from 5 mm to 3 cm in width from 3 mm to 2 cm and in depth from 10 mm to 22 mm. (Hill and Sachs 1940)
A number of special projections have been describe to enhance the view of the Hill Sachs defect. (Adams 1950; Didiee 1930; Hall et al 1959; Hermodsson 1934; Hill and Sachs 1940; Moseley 1961; Oppenheim et al 1985; Pavlov Warren Weiss et al 1985; Symeonides 1972) Two of these views bear special mention.
The Stryker notch view
The patient is supine on the table with the cassette placed under the shoulder. (Hall Isaac and Booth 1959) The palm of the hand of the affected shoulder is placed on top of the head with the fingers directed toward the back of the head. The elbow of the affected shoulder should point straight upward. The x-ray beam tilts 10 degrees toward the head centered over the coracoid process (see figure 17). This technique was developed by William S. Stryker and reported by Hall and coworkers. (Hall Isaac and Booth 1959). They stated that they could demonstrate the humeral head defect in 90 per cent of 20 patients with a history of recurring anterior dislocation of the shoulder.
The apical oblique view
Garth and coworkers (Garth Allman and Armstrong 1987; Garth et al 1984) described the apical oblique projection of the shoulder (see figure 18). In this technique the patient sits with the scapula flat against the cassette (as for the anteroposterior view in the plane of the scapula). The arm may be in a sling. The x-ray beam is centered on the coracoid and directed perpendicular to the cassette (45 degrees to the coronal plane) except that it is angled 45 degrees caudally. The beam passes tangential to the articular surface of the glenohumeral joint and the posterolateral aspect of the humeral head. This view is likely to reveal both anterior glenoid lip defects and posterior lateral impression fractures of the humeral head.
The incidence of the Hill Sachs defect reported depends on both the radiographic technique and the patient population. Symeonides (Symeonides 1972) reported the humeral head defect in 23 of 45 patients who had recurrent anterior dislocations of the shoulder. However at the time of surgery he could confirm only 18 of 45.
Eyre-Brook (Eyre-Brook 1971) reported an incidence of the Hill Sachs defect of 64 per cent in 17 recurrent anterior dislocations and Brav (Brav 1960) recorded a rate of 67 per cent in 69 recurrent dislocations. Rowe (Rowe et al 1977) noted the defect in 38 per cent of 125 acute dislocations and in 57 per cent of 63 recurrent dislocations. Adams (Adams 1948) noted that the defect was found at the time of surgery in 82 per cent of 68 patients. Palmer and Widen (Palmer and Widen 1948) found the defect at surgery in all of 60 patients.
Calandra and coworkers (Calandra et al 1989) prospectively studied the incidence of Hills-Sach lesions using diagnostic arthroscopy. In a young population of 32 patients with a mean age of 28 years the frequency of this lesion was 47% for initial anterior shoulder dislocations.
Danzig Greenway and Resnick (Danzig et al 1980) reported that in cadaveric and clinical studies no single view will always reveal the humeral head compression fracture. Pavlov and coworkers (Pavlov Warren Weiss et al 1985) and Rozing and associates (Rozing et al 1986) found that the Stryker notch view taken in internal rotation best revealed the posterolateral humeral head defect (see figure 14).
The demonstration of a posterior lateral humeral head defect strongly indicates that the shoulder has been subject to a traumatic anterior dislocation. When these factors are already known--for example in a 17-year-old whose recurrent anterior dislocations began with a well-documented abduction-external rotation injury in football--it is not necessary to spend a great deal of effort demonstrating the humeral head defect because (1) it is very likely to be present even if not seen on the radiographs and (2) the existence of such a lesion does not in itself alter our management of the patient.
Glenoid changes
Standard radiographs may reveal a periosteal reaction to the ligamentous avulsion at the glenoid lip or a fracture (see figure 19) erosion or new bone formation at the glenoid rim. Modifications of the axillary view may help the identification of glenoid rim changes. Rokous (Rokous et al 1972) and colleagues described what has become known as the "West Point" axillary view. (Rockwood 1984) In this technique the patient is placed prone on the x-ray table with the involved shoulder on a pad raised 7.5 cm from the top of the table. The head and neck are turned away from the involved side. With the cassette held against the superior aspect of the shoulder the x-ray beam is centered at the axilla 25 degrees downward from the horizontal and 25 degrees medial. The resulting x-ray is a tangential view of the anteroinferior rim of the glenoid (see figure 20). Using this view Rokous and associates demonstrated bony abnormalities of the anterior glenoid rim in 53 of 63 patients whose histories indicated traumatic instability of the shoulder. Cyprien and coworkers (Cyprien Vasey and Burdet 1983) demonstrated lessening of the glenoid diameter and shortening of the anterior glenoid rim in shoulders with recurrent anterior dislocation. Blazina and Satzman (Blazina and Satzman 1969) also reported anteroinferior glenoid rim fractures seen on the axillary view in nine of their cases.
Special radiographic techniques
Although pathology can be seen with additional radiographic views (Green and Christensen 1994; Minkoff and Cavaliere 1993; Palmer and Caslowitz 1995; Rafii et al 1993) CT arthrography (Braunstein and O'Conner 1982; Cramer et al 1982; El-Khoury et al 1986; Kelley 1954; Kleinman et al. 1984; McGlynn et al 1982; McMaster 1986; Rafii et al 1986; Rafii et al 1987; Shively and Johnson 1984) fluoroscopy (Norris 1984) or MRI these additional tests are rarely cost-effective in the clinical evaluation and management of shoulders with characteristic traumatic instability. (Engebretsen and Craig 1993; Liu and Henry 1996) While CT evidence of labral or capsular pathology is unlikely to change the management of the shoulder contrast computerized tomography may help document the flattening of the anteroinferior glenoid concavity due to loss of articular cartilage. CT may also be useful in defining the magnitude of bone loss when sizable humeral head or glenoid defects are suggested on plain radiographs. (Gould et al 1985; Seltzer and Weissman 1985) When previous glenoid bone blocks have been carried out or hardware inserted CT is useful for examining the possibility of their encroachment on the humeral head. (Cramer 1882; Cramer Von and Kramps 1982; Danzig et al 1982)
Although many articles have been written regarding the use of MRI in imaging the unstable shoulder (e.g. Chandnani et al 1993; Gross et al 1990; Iannotti et al 1991; Kiett et al 1988; Meyer and Dalinka 1990; Neumann et al 1991; Palmer and Widen 1948; Richards et al 1994; Runkel et al 1993; Vellet et al 1991) the clinical usefulness of this examination awaits definition. Iannotti et al (Iannotti Zlatkin Esterhai et al 1991) reported the sensitivity and specificity of MRI in the diagnosis of lateral tears associated with glenohumeral instability were 88 and 93% respectively. However in a blinded study Garneau et al (Garneau et al 1991) found that it was insensitive and nonspecific for labral pathology. Even if MRI reliably yielded this information it is unclear how it would be cost-effective in the management of the patient: patients with refractory instability would be considered for surgery with or without such data.
Rotator cuff imaging
In a patient whose onset of traumatic instability occurred after age 35 there may be evidence on history and physical examination of rotator cuff pathology. Particular concern arises if weakness of external rotation or elevation persist longer than a week or so. In these situations preoperative imaging of cuff integrity may play an important role in surgical planning: the approach for rotator cuff repair is quite different than the approach for the repair of an anterior inferior capsular lesion. Arthrography ultrasound or MRI may be useful in this situation.
Electromyography
Electromyography may be helpful in the evaluation of the patient with recurrent traumatic instability if the history and physical examination suggest residual brachial plexus lesions.
Arthroscopy
Diagnostic arthroscopy is not a necessary prelude to open surgical repair of documented recurrent traumatic instability. While it uncommonly changes the surgical approach shoulder arthroscopy has helped define some of the pathology associated with recurrent instability. Such lesions include labral tears capsular rents humeral head defects and rotator cuff defects. (Andrews et al 1983; Carew-McColl 1980; Frizziero 1981; Garth Allman and Armstrong 1987; Ha'eri and Maitland 1981; Hintermann and Gachter 1994; Johnson 1980; Lilleby 1982; McMaster 1986; Mital 1980; Older 1976; Parisien 1983; Wiley and Austwick 1982; Wiley and Older 1980; Zizzi et al 1981)
A classification of anterior labral "Bankart" lesions was proposed by Green and Christensen. (Green and Christensen 1995) In 37 cases they described the arthroscopic appearance common to five separate groups. Type I is the normal intact labrum. Type II is a simple detachment of the labrum from the glenoid. Type III is an intrasubstance tear of the glenoid labrum. Type IV is a detachment of the labrum with significant fraying or degeneration and Type V is a complete degeneration of absence of the glenoid labrum.
Neviaser found that occasionally the anterior labroligamentous periosteal sleeve is avulsed from the supporting anterior inferior ligamentous and labral structure. (Neviaser 1993)
Habermeyer and Gleyze found that shoulders with more than five recurrent dislocations were found to have anterior articular cartilage erosion. (Gleyze and Habermeyer 1996) Harryman noted labral damage in all cases treated for recurrent anterior traumatic instability and significant articular erosion to subchondral bone in 20%. (Harryman 1996)
Other lesions may be associated with Bankart lesions. Snyder et al (SnyderBanasKarzel 1995) and Warner (Warner et al 1994) found the association of superior labral detachment and Bankart lesions.
Wolf reported that 6 of 64 patients with anterior instability had avulsion of glenohumeral ligaments from the humerus while 47 had true Bankart lesions (73.5%). (Wolf et al 1995)
Arthroscopy also reveals defects in the articular cartilage of the posterior lateral humeral head which would not be detected on radiographs.