Soft Tissue Masses: Diagnosis and Surgery for Benign and Cancerous Tumors (Sarcoma)
In this article:
- Basics of soft tissue masses
- Incidence and Acquisition
- Symptoms & Effects on Daily Life
- Risk Factors
- Prevention
- Diagnosis
- Treatment
- Additional Resources
- Research
- Summary of soft tissue masses
Basics of soft tissue masses
Soft tissue tumors are cell growths that emerge nearly anywhere in the body: in tendons, muscles, ligaments, cartilage, nerves, blood vessels, fat, and other tissues. Patients commonly refer to these masses as lumps or bumps.
See Figures 1 and 2. Figure 1 illustrates the appearance of a patient who presented with a benign soft tissue mass in the arm. Figure 2 illustrates the appearance of a sarcoma in the thigh. Note the large size of the mass along with the overlying skin changes in Figure 2. Click the images below to enlarge.
Soft tissue tumors can be cancerous or benign. Benign masses are thought to occur 10 times more frequently than cancerous growths (referred to medically as sarcomas). Generally these growths are roughly round in shape, but they also can be or elliptical or elongated like a sausage. Masses greater than 5 cm (2 inches) carry the highest risk of being malignant and merit a medical evaluation.
They can feel firm or soft. Benign masses are more likely to be painful to the touch, such as with an abscess. Benign tumors also tend to grow more slowly, and many are smaller than 5 cm (2 inches) at their longest point.
Sarcomas (cancerous growths) more often are painless. Cancerous masses are more likely to grow rapidly, and to have fingerlets or satellite lesions around them.
According to the National Cancer Institute, about 43 percent of sarcomas occur in arms and legs; 34 percent occur in and around internal organs; 10 percent occur in the chest and back region; and 13 percent occur in other locations.
The masses – benign or cancerous – come to clinical attention more quickly when they are located in the arms and legs, as opposed to the chest or abdomen, because less room exists in arms and legs for such masses to be mistaken for other bodily structures.
Immediate medical attention
A newly found soft tissue mass is rarely an emergent condition. Not all soft tissue masses require surgery, and removal of a known benign tumor can be safely delayed. However, any suspected (cancerous growth) should be worked-up and biopsied as soon as possible so further treatment can be rendered.
Any newly discovered mass of unknown origin that is growing should be evaluated by a specialist. Any sprain or hematoma (bruise) that lasts longer than six weeks merits additional medical scrutiny for the possibility of sarcoma (cancerous growth).
Facts and myths
Depending on its location, a soft tissue mass often is initially misdiagnosed as a muscle sprain, hematoma, or old trauma that will heal in time. Such misperceptions can contribute to delayed diagnoses of soft tissue tumors – often as long as three to six months after the patient's initial discovery of a bump or lump. Because the tissue masses often cause no pain, people tend to think the bumps are not harmful.
Incidence and Acquisition
Incidence
Some 10,000 new soft tissue and bone sarcomas (cancerous growths) are diagnosed annually in the United States. Benign soft tissue tumors are discovered at a significantly higher rate than sarcomas.
Soft tissue tumors affect every segment of the population. However, sarcomas occur more often in children and young adults, and men have a slightly higher rate of sarcoma than women.
Some sarcomas are more prevalent among specific populations. For example, synovial sarcoma is more often found in young adults.
In the vast majority of cases, a soft tissue tumor is a spontaneous occurrence without a well-defined cause.
Acquisition
Evidence suggests that some genetic disorders and mutations predispose people to benign and cancerous soft tissue tumors. Exposure to radiation and environmental carcinogens has been associated with soft tissue tumors. Kaposi’s sarcoma is an example of an infection-induced soft tissue tumor –resulting from a type of herpes in patients who also have HIV.
Most people with a soft tissue tumor do not have a well-defined cause for their tumor. Lifestyle factors, injury, and infection have not been consistently proven to cause soft tissue tumors in the majority of cases.
Genetics
Rare genetic abnormalities and disorders can predispose people to benign and malignant soft tissue tumors. For example, a gene linked to neurofibromatosis – nerve-sheath tumors – has shown likelihood to become cancerous.
Conditions with similar symptoms
A hematoma, cyst from arthritis, or swelling from a sprain or strain might be confused with a soft tissue tumor.
Causes
The cause of most soft tissue tumors is not known. Evidence suggests that some genetic disorders and mutations predispose people to benign and cancerous soft tissue tumors. Exposure to radiation has a strong association with the development of a sarcoma (cancerous growth). There are weak associations of soft tissue tumors with exposure to environmental carcinogens.
Effects
A soft tissue tumor grows, slowly or quickly, in the body, based on its etiology. Generally, soft tissue tumors grow in a round orientation, though some can grow more oval or sausage-shaped. Most such growths remain within borders of fascia tissue, though they can cross such boundaries as they grow.
They can grow around bones, muscles, blood vessels, nerves, and other structures, causing compression or change in function of those structures.
Occasionally, a sarcoma (cancerous growth) can spread (metastasize) to other parts of the body, usually the lungs.
Symptoms & Effects on Daily Life
Initial symptoms
Soft tissue tumors offer little warning. They can emerge as a lump or bump slowly or quickly in any part of the body.
The emergence of the mass itself is the most common symptom. It is usually round or oval in its dimensions. It often is painless, causing notice or discomfort only in cases when it compresses a nerve or irritates other tissue. A rapid rate of increase in size of a mass suggests the possibility of malignancy.
Progression
Depending on the tumor’s etiology, it can grow quickly or slowly. Some soft tissue masses that are initially benign can transform into malignancies. This is often heralded by an abrupt increase in the size of a previously quiescent mass. Research suggests that a malignant mass that emerges in an arm or leg is usually greater than 5 cm (2 inches) in size and deep-seated (often in muscle).
Prognosis
Most soft tissue tumors emerge spontaneously. They merit attention because they could be cancerous. A sprain or hematoma that lasts longer than six weeks merits additional medical scrutiny for the possible presence of a soft tissue tumor.
The risk of recurrence is related to the type of tumor, the adequacy of initial surgical excision, and the tumor’s location. Rarely, people are genetically predisposed to have soft tissue masses (e.g., neurofibromatosis, in which tumors grow on nerves).
Lethality
Most soft-tissue tumors are benign. Large masses are more cause for worry. Patients who notice a mass more than 5 cm (2 inches) at its longest point, or which is painful to the touch, should consult a physician.
A soft-tissue sarcoma (cancerous growth) can be a lethal disease. For instance, synovial sarcoma is an aggressive cancer that accounts for 7 percent to 10 percent of soft-tissue sarcomas, and usually develops in the arms or legs of young adults. Research shows that as few as 25 percent of those patients with disease that has metastasized, or spread, to other parts of the body survive five years.
Pain
The majority of soft tissue masses are painless -- unless they are irritating a nerve nearby – and this is a primary reason why many masses are not diagnosed until they have developed significantly in size. Soft tissue masses may cause skin discoloration if blood flow increases to the region or if veins are distended, but usually skin around the mass retains its normal color.
Debilitation
Prompt and accurate diagnosis is important to help avoid debilitating complications. Soft tissue tumors often are not physically debilitating, at least initially, and this contributes to their ability to grow undetected. Patients who notice a mass more than 5 cm (2 inches) at its longest point, or which is painful to the touch, should consult a physician.
A sarcoma (cancerous growth) could result in amputation of an arm or leg or functional loss of a limb. A benign tumor could, in some cases, be debilitating too. For example a soft tissue mass deep in the pelvis could impede the function of an organ, such as the bowel, or interfere with local nerves or blood flow.
Comfort
In some cases, a soft tissue tumor could cause a patient discomfort, especially if there is local irritation of a nerve or blood vessel. A tumor on someone's foot could impede his or her ability to wear shoes and walk comfortably. A mass pressing against the stomach could cause discomfort with the patient's digestion, and similarly, a mass next to the rectum could cause constipation.
Curability
Some of the 50 subtypes of sarcomas (cancerous growths) are curable with a combination of surgery, chemotherapy and/or radiation. Other sarcomas are more aggressive and more challenging to treat.
Fertility and pregnancy
In most cases, a soft tissue tumor in and of itself will not impede one’s ability to have children or get pregnant. Sometimes, chemotherapy can interfere with the function of the ovaries or testes. Therefore, any patient planning for a pregnancy should have a thorough discussion with her medical oncologist.
Independence
The body has an amazing capacity to recover from many surgeries in which soft tissue masses are removed. In many areas of the body, muscles are redundant and can compensate well for removal of muscle or soft tissue. In some cases, however, a soft tissue tumor could affect a patient's independence; for example, surgeons might have to remove a nerve to effectively remove a sarcoma (cancerous growth), requiring a patient to wear a brace or follow a program of physical therapy to regain full mobility. Sarcomas that result in amputation of a limb could change a patient's independence dramatically. Thankfully, modern prosthetic devices have been particularly successful for restoration of independence in the amputee population.
Mobility
Depending on its location, a soft tissue tumor could affect a patient's mobility. For example, a tissue mass on a patient's foot or pressing against a patient's nerve could reduce mobility. Similarly, surgeons might have to remove a nerve or muscle to effectively remove a sarcoma (cancerous growth), which could compromise mobility.
Daily activities
A soft tissue tumor could inhibit or change a patient's ability to maintain daily work tasks or activities. A tumor on a patient's finger or hand could impede typing, for instance; a tumor that involves a nerve could cause a patient to reduce his or her activities because of pain or functional deficit.
Energy
A soft tissue mass in and of itself usually does not cause fatigue or changes in metabolism. A newly found mass may elicit patient anxiety which may lead to fatigue.
Chemotherapy treatment for a sarcoma (cancerous growth) could cause a patient fatigue, as well.
Diet
Soft tissue tumors typically do not require changes in diet.
Relationships
A sarcoma (cancerous growth) or benign tissue mass may have implications for social relationships. For example, a tissue mass that affects a patient's sexual function could affect social relationships.
People who are diagnosed with soft tissue tumors are often anxious because of the presence of their mass and need strong social support to help them through the diagnosis and possible treatment. It is important to remember that treatment helps the majority of patients with these tumors, enabling individuals to live full, active lives.
Other impacts
Nerve or muscle disability might result from a surgeon’s resecting of those tissues to remove a tumor. Rarely, an amputation is needed to effectively treat a sarcoma (cancerous growth). Research suggests that children have an easier time adjusting to an artificial limb than adults.
Communicability
Soft tissue tumors are not contagious.
Risk Factors
Lifestyle risk factors
Lifestyle and diet are not thought to play a role in the emergence of soft tissue tumors – benign or cancerous.
Injury & trauma risk factors
Historically there have been many case associations between trauma and soft tissue masses, but data does not support trauma as the cause of such masses. More likely is that the trauma drew medical attention to the existing tissue mass.
One exception would be a ganglion cyst, a common, benign fluid-filled soft tissue mass that can be caused by injury. A ganglion cyst might develop after a knee injury, for instance. Such cysts usually move about more freely and are much softer than a sarcoma (cancerous growth).
Prevention
Soft tissue tumors cannot be prevented, per se, but any discovered mass of unknown etiology that is growing should be evaluated by a specialist. Any sprain or hematoma that lasts longer than six weeks merits additional medical scrutiny.
Anatomy
According to the National Cancer Institute, about 43 percent of sarcomas (cancerous growths) occur in the arms and legs; 34 percent occur in and around internal organs; 10 percent occur in the chest and back region; and 13 percent occur in other locations.
The masses – benign or cancerous – come to clinical attention more quickly when they are located in the arms and legs, as opposed to the chest or abdomen, because less room exists in arms and legs for such masses to be mistaken for other bodily structures.
Secondary effects
Depending on the tumor’s etiology and location, it can displace or compress nerves, blood vessels, and other bodily structures, affecting their function.
Diagnosis
Patients presenting with soft tissue masses are evaluated and their clinical history taken. Diagnostic tests might include X-ray, magnetic resonance imaging (MRI), positron emission tomography (PET) scan, computed tomography (CT) scan, bone scan, and angiogram.
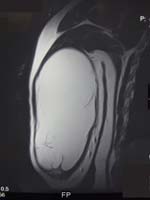
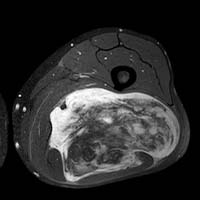
See Figures 3 and 4 below. Figure 3 illustrates the appearance of a soft tissue mass on MRI. This “fatty mass” in light color is a lipoma. Figure 4 illustrates the appearance of a sarcoma (cancerous growth) in the back of a person’s thigh. Click the image to enlarge
With this information in hand, the physician would biopsy the mass to diagnose its etiology. If a biopsy is needed, the surgeon who does the biopsy should be the person who will remove the mass. If the mass is benign, often surgeons will remove it immediately, but it may not require removal. If the mass is malignant, it likely will be treated with surgery, chemotherapy or radiation (or a combination thereof).
Diagnostic tests
Patients presenting with soft tissue masses are evaluated and their clinical history taken. Diagnostic tests might include X-ray, magnetic resonance imaging (MRI), positron emission tomography (PET) scan, computed tomography (CT) scan, bone scan, and angiogram.
See Figures 5 and 6 below. Figure 5 is the appearance of a soft tissue mass on the chest wall. Figure 6 is a CT scan and was necessary to precisely localize the area of the mass. The mass was found to arise from a rib.
These tests indicate the tissue mass’ orientation within and across surrounding structures, such as nerves and bones, and the mass’ aggressiveness and any suggestion that it has metastasized, or will.
Effects of diagnosis tests
The imaging required to work-up a soft tissue tumor is fairly painless. If contrast is used for a CT scan, then an intravenous line may be needed. Some people get claustrophobic in the MRI scanner machine, and need medicine to prevent anxiety. A biopsy of a soft tissue tumor causes minimal pain and discomfort.
Soft Tissue Masses: Your Health Care Team
Soft tissue masses can emerge anywhere in the body, and specialists cross the spectrum of physician expertise. Orthopedic oncologists tend to perform resections from the arms and legs, pelvis, spine and occasionally the chest wall; general surgical oncologists tend to operate when tumors are located in the abdomen or pelvis. Otolaryngologists and/or neurosurgeons typically perform surgery to remove head and neck tumors. Spinal specialists often assist with spinal surgeries.
Soft Tissue Masses: Finding a doctor
Surgical care of soft tissue tumors should be performed in specialty centers well-practiced in sarcoma (cancerous growth) surgeries. There is good evidence in the medical literature to support this idea.
Surgeons remove some 40,000 soft tissue masses every year in the United States; 10,000 of these are sarcomas – a relatively low number, compared with incidences of breast cancer or prostate cancer, for example. Given this, relatively fewer surgeons in the United States specialize in the care of soft tissue tumors, malignant or benign.
Patients should seek out a surgeon who has a high volume practice and much experience in treating soft tissue tumors. The American Academy of Orthopedic Surgeons or the Musculoskeletal Tumor Society are reliable resources for identifying surgeons with the above-mentioned qualifications.
Treatment
Upon diagnosis, a soft tissue mass can be observed or prepared for removal from the patient’s body.
Benign fat tumors (lipoma), for example, can be observed, rather than removed, with a recommendation of routine surveillance for the patient – an MRI every six to 12 months, depending on the tumor’s location. Patients have lived for decades with slow-growing benign tumors instead of having them removed immediately.
If a sarcoma (cancerous growth) is diagnosed, doctors recommend expeditious treatment involving surgery, chemotherapy, radiation therapy or a combination thereof.
For any soft tissue tumor, the surgeon's goal is to remove all of the tumor. With cancerous tumors, surgeons more aggressively remove surrounding tissue. But doing so may leave a greater resulting soft-tissue defect for the patient, requiring the expertise of a reconstructive surgeon to help fill or make the area more cosmetically appealing.
The challenge of surgery depends largely on the tumor's location. Proximity of blood vessels, nerves and other vital tissues contribute to a surgery's technical difficulty. The tumor's size and its etiology contribute to the length of the procedure and the surgeon's ability to remove all of the tumor.
Self-management
Patients cannot treat soft tissue tumors. If a patient suspects a soft-tissue tumor, he or she could take the initiative to schedule an appointment with a family doctor.
Health care team
Soft tissue masses can emerge anywhere in the body, and specialists cross the spectrum of physician expertise. A fundamental principle of soft tissue tumor management is that the biopsy and surgery be performed by the same individual. Orthopedic oncologists tend to perform resections from the arms and legs, pelvis, spine and occasionally the chest wall; general surgical oncologists tend to operate when tumors are oriented in the abdomen or pelvis. Otolaryngologists and/or neurosurgeons typically perform surgery to remove head and neck tumors. Spinal specialists often assist with spinal surgeries. Vascular surgeons may be necessary if reconstruction of a an artery is necessary.
Pain and fatigue
Acetaminophen, nonsteroidal anti-inflammatory drugs, and, infrequently, narcotic pain medicines may be used for relief from pain caused by soft tissue tumors.
Diet
Diet is not known to be able to beneficially treat a soft tissue tumor.
Exercise and therapy
Exercise, therapy, rest and posture changes are not known to help treat a soft tissue tumor.
Medications for soft tissue masses
Most of the times, medications are not called for in treating benign soft tissue masses. For tissue masses diagnosed as sarcomas (cancerous growths), chemotherapy medications may be used in treatment. Hormonal therapy or non-steroidal anti-inflammatory medicine have been used with varying results to treat desmoids (benign, locally aggressive fibrous tumors).
Surgery for Soft Tissue Masses
When performed by an experienced surgeon, excision/resection of a soft tissue mass is very effective. Benign soft tissue tumors are treated with surgery alone. In cases of sarcoma (cancerous growth), surgery often is indicated as the best potential resolution, often in concert with chemotherapy and radiation treatment.
For a patient facing such surgery, a comprehensive clinical evaluation of the patient should have been done one or two visits beforehand. Patients should educate themselves about surgical options and risk, and their doctor's experience, in advance of surgery.
Many soft tissue resections require patients to stay overnight afterward, at least one or two days and potentially longer, depending on the invasiveness of the procedure. Many patients have drains inserted with surgery so edema fluid does not build up under the wound. Postoperatively, hospital staff monitors the drainage as well as signs of infection and healing. Many patients receive oral antibiotics to prevent infection, and receive pain medication orally or by IV for a day or two after surgery.
Patients who have been treated with radiation before surgery are more vulnerable to infection afterward, as radiation can affect the integrity of the skin, making wound healing more problematic.
Patients may have residual discomfort from surgery, and take anti-inflammatory or pain medication orally for a week or two afterward. Most patients can manage pain well after surgery.
Depending on the location of surgery, patients may need to go therapy to fully recover to their preoperative strength and activity level. Tumors that involve a major portion of muscle in the lower leg, for example, could need weeks or months of a physical therapy program. Some patients may require amputation of a limb if the soft tissue tumor cannot be safely removed otherwise. Those patients could face a prolonged recovery.
Joint aspiration
Joint aspiration is the process of removing some fluid from the sore joint(s). It is not indicated as a treatment for soft tissue tumors.
Splints or braces
In cases in which a tumor is excised from a leg and adversely affects musculature that enables a patient to walk, the patient might benefit from use of a brace or splint in rehabilitation.
Alternative remedies
Some practitioners and patients suggest that yoga, acupuncture, and relaxation techniques may be integrated with more traditional approaches to yield a more holistic healing.
Social impacts
Chemotherapy and radiation treatment for a sarcoma (cancerous growth) can have side effects such as lethargy, hair loss and nausea that likely would impact a patient’s energy for social interactions.
Removal of a large tumor also could leave a visible deficit, or sunken area, which might not entirely be repairable by reconstructive surgery. Such a deficit might affect a patient’s outlook or heighten a feeling of self-consciousness.
The diagnosis of a sarcoma involves long-term follow-up with a physician. Some patients need to travel long distances to see their specialist. This may pose challenges to one’s personal life.
Long-term management
If not removed entirely by surgery, the growth of benign tumors should be monitored regularly by the patient and every six months to a year by the physician.
In cases of sarcoma (cancerous growth), patients should have regular rechecks of their condition to monitor whether the cancer has metastasized or recurred. Often tumors are treated with weeks or months of radiation to combat their likelihood of recurrence. The risk of recurrence is related to the type of tumor, the adequacy of initial surgical excision, and tumor location.
Patients for whom safe removal of sarcoma necessitated amputation of a limb could face a prolonged therapeutic recovery.
Unproven remedies
Naturopathic approaches for treatment of soft tissue tumors are largely unproven.
Strategies for coping
A sarcoma’s ability to go undetected in the body is troublesome, even after the growth is discovered. Initially, the patient might struggle with not knowing whether a soft tissue tumor is cancerous or benign. After surgery, a patient might feel emotionally exhausted from worry about whether to anticipate recurrence of such a tumor.
A patient might take comfort in knowing that three of every four soft tissue masses discovered are benign. Nevertheless, a majority of patients express fear and anxiety with the recognition of such masses.
Patients who experience great anxiety in learning of a cancerous tumor, or learning of a benign tumor in a dangerous location in the body, might seek help from family, friends, a mental health professional, a hospital’s pastoral care group, or through nontraditional therapies such as reiki.
Asking for help
Cancer patients and their families should learn as much as they can about the disease. Sometimes talking with a family member or friend can provide much needed emotional support. Working with a counselor, psychologist, or social worker helps some people with cancer to develop better coping skills.
Support groups have been a source of help for thousands of cancer patients.
Sarcoma Alliance, Sarcoma Foundation of America, and Northwest Sarcoma Foundation are a few of the several organizations that offer support networks for patients coping with cancerous soft tissue masses.
Work
Most people with a soft-tissue tumor can continue to work. Doctors and work supervisors should be able to help people make any needed changes to relieve discomfort. This could include adjusting a work area or reducing the amount of time spent doing particular tasks. An occupation therapist can help find ways to modify activities or suggest tool modifications.
Family and friends
Children may feel angry, sad or self-conscious about having a tumor. Acceptance and settling into a routine will benefit everyone in the family.
When parents are first told that their child has cancer, for example, they might feel shocked, numbed, or disbelieving. They might also feel guilty, and ask themselves if something they did or didn't do caused their child's condition.
The child with a tumor may feel "hurt" by an illness that isn't their fault, blame parents for the illness, adopt a "why me?" attitude, engage in self-pity or become angry. They may resent other children who are well, including brothers and sisters.
Other children might feel left out and resentful because of the amount of time and attention the child with cancer requires. Or they may feel guilty, as if their normal "bad thoughts" towards their brother or sister had somehow caused the illness.
Children might over-identify with the brother or sister with special needs. Some feel a pressure to achieve or make up for what their brother or sister can no longer do. Others want to involve themselves in care-giving – to the point where they give up their own normal activities. In these cases, try to help siblings find other ways to deal with their feelings. Whenever possible, brothers and sisters should be allowed to settle their own differences. Siblings should be encouraged to talk with peers who live in homes with similar concerns. The key to dealing with all these emotions is to talk about them with one another.
Children should be encouraged to learn as much as they can about cancer and their treatment program. Older children can be responsible for taking medications on time, reporting any medication side effects to you, and following an exercise program. This may help prepare them for the change to adult health-care.
Children with cancer should not be overprotected. They might become too dependent if their parents do everything for them or if the parents keep them from tasks they are capable of doing. Parents should not be manipulated into allowing activities that shouldn't be done, but should compromise when possible. Consistency will help children learn what is expected.
Parents should plan special time to spend alone with their spouse, or with the entire family. When their child first becomes ill, they may set aside relationships with other family members. It is important, however, to continue to talk and spend time with all family members.
Adaptive aids
Patients for whom safe removal of sarcoma (cancerous growth) left them less mobile might find aid in crutches, braces, a cane, or a walker – or if a leg was amputated, in prostheses. A wheelchair may be necessary short-term if walking ability has been affected or for elderly patients who have difficulty walking. Wheelchairs may be required by some people. Special reaching devices are available to ensure that patients can reach whatever they need.
Stress
Support from family, friends, or a support group often helps patients cope with stress related to a soft tissue tumor. Sarcoma (cancerous growth) patients often find it helpful to speak to other individuals who have been through treatment for this rare diagnosis. Sarcoma Alliance, Sarcoma Foundation of America, and Northwest Sarcoma Foundation are among the organizations that can put patients in touch with other sarcoma survivors.
Additional Resources
- Fred Hutchinson Cancer Center
- Cancer Lifeline in Seattle
- The Sarcoma Alliance
- The Northwest Sarcoma Foundation
- The Sarcoma Foundation of America
Research
Condition research
Benign tumors do not always require removal or further treatment. With cancerous tumors, a significant volume of ongoing research studies treatment methods. Novel chemotherapy drugs are being tested in multicenter clinical trials, and researchers are trying to identify molecular targets for sarcomas (cancerous growths) – which may assist with designing drugs aimed at curing this cancer. Metabolic imaging such as PET (Positron emission tomography) scanning is opening avenues to assess tumor response to chemotherapy and to identify those tumors that are most aggressive.
Pharmaceutical research
Many new drugs are being tested in clinical trials to treat soft tissue tumors. These trials take time especially because sarcomas (cancerous growth) are rare. Much effort is being focused on drugs to treat those patients with very advanced disease – disease that has metastasized.
Non-surgical research
Different types of radiation and methods for delivering radiation are being tested to determine how to best treat soft tissue tumors.
Surgical research
There is ongoing investigation about how to optimally treat soft tissue tumors from a surgical perspective. Surgeons are trying to identify novel ways to maximize tumor control, without compromising function or survival. The concept of what constitutes the optimal surgical margin for specific tumor subtypes is currently under debate.
Summary of soft tissue masses
- Soft tissue masses are found to be benign in about three out of four instances. Such masses can emerge in almost any site in the body.
- Delay in diagnosis of soft tissue tumors is common. A sprain or hematoma that lasts longer than six weeks merits additional medical scrutiny for the possibility of soft tissue tumor.
- Surgical care of soft tissue tumors should be performed in a multidisciplinary specialist center.
- Any newly discovered tissue mass that is growing should be evaluated by a medical specialist. Not all soft-tissue masses must be removed, but any should be suspected of cancerous potential until proven otherwise.
- Many sarcomas (cancerous growths) go undetected until they are quite large, and therefore become more difficult to treat.
127