Overview
Basics of knee arthritis
Many kinds of arthritis can affect the knee joint but by far the most common is osteoarthritis which some people call "degenerative joint disease."
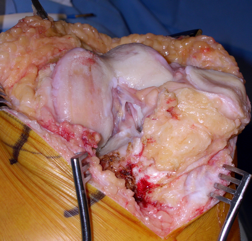
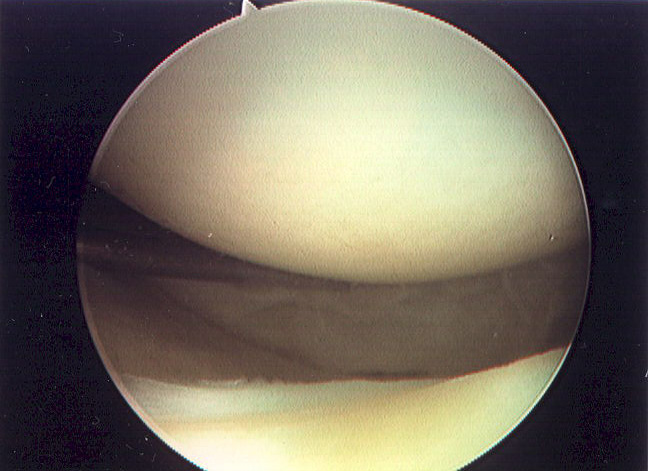
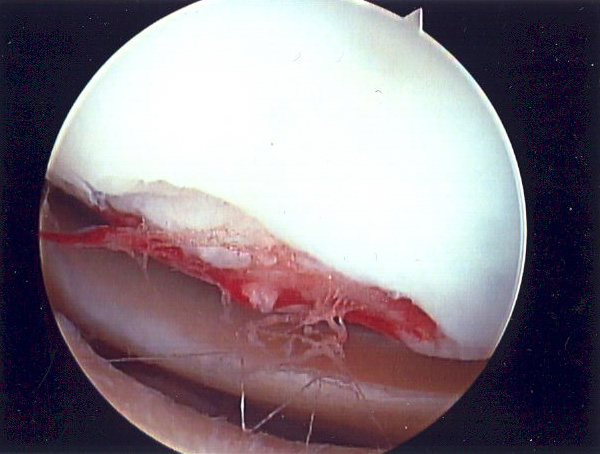
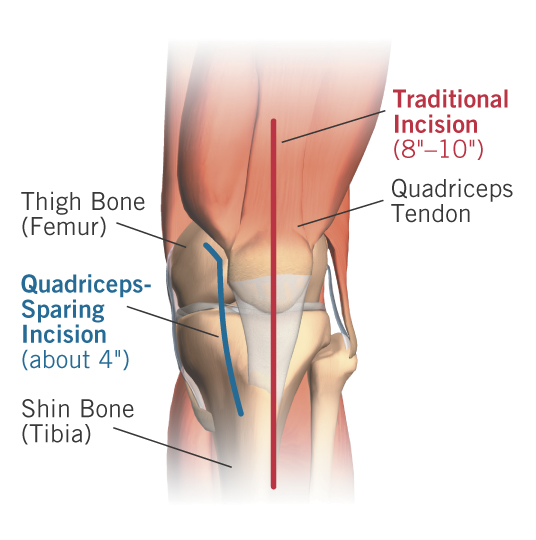
This occurs when the joint surface cartilage (also called hyaline cartilage or articular cartilage) becomes worn away leaving the raw bone beneath exposed (See Fig 1). The cartilage normally serves as a “pad” or a bearing in the joint and under normal conditions the cartilage bearing is even slicker than a hockey puck on ice. When the bearing wears away the result is a roughed joint surface that causes the pain and stiffness that people associate with osteoarthritis (See Fig 2 and Fig 3). and for most patients who have only mild arthritis the pain can be managed with simple things such as ice rest activity modifications pills or joint injections. However if the arthritis becomes severe (See Fig 4 and Fig 5) the pain may not respond to those kinds of interventions. Patients with severe arthritis sometimes can benefit from joint replacement surgery either partial (unicompartmental) knee replacement or total knee replacement (See Fig 6) which now can be done using a minimally-invasive quadriceps-sparing approach that can significantly shorten the recovery and decrease the pain following surgery.
joint surface cartilage
arthritis of the knee
from knee arthritis
knee replacement prosthesis
Immediate medical attention
Osteoarthritis of the knee is not an emergency. It can however result in disturbing “flare ups ” with increased pain and swelling. Many patients who experience a sudden flare-up will go to the doctor for care and for many patients this apparently "acute" set of symptoms will result in the diagnosis of this chronic condition.
Facts and myths
MYTH: Osteoarthritis of the knee is not usually the result of “overuse.”
True. There have been studies of long-distance runners that show that they are not more likely to get arthritis than more sedentary individuals. However people in occupations that require extreme and repeated heavy exertions (such as farmers) experience higher rates of osteoarthritis.
MYTH: Osteoarthritis of the knee is a “normal result of aging.”
True. Studies show aging have more "doctor-diagnosed" arthritis.
MYTH: Osteoarthritis of the knee is just “aches and pains.”
False. It is a condition whose biology x-ray appearance (See Fig 4) and clinical symptoms are defined.
MYTH: Not much can be done for osteoarthritis of the knee.
False. In fact there are exercise programs that can alleviate the pain in mild arthritis a variety of medications and injections can be helpful for moderate arthritis and severe arthritis of the knee is very commonly successfully treated with knee replacement surgery (See Fig 6). New minimally invasive approaches appear to decrease the recovery time from this operation.
MYTH: Women have more “doctor-diagnosed” arthritis than men.
True. Studies show women also report greater activity and work limitations, greater psychological distress and more severe joint pain than their male counterparts.
Symptoms & Diagnosis
Prognosis
Osteoarthritis of the knee is a serious condition. Osteoarthritis is the most common of the more than 100 kinds of arthritis and the knee joint is the most commonly affected large joint in the body. Osteoarthritis of the knee results in pain stiffness and joint deformity (See Fig 5) which can affect one’s ability to walk work and enjoy life. It is a chronic disease meaning that it takes months to years to appear; while it is not “curable ” it most certainly is treatable using activity modifications medications injections and if those interventions don’t work knee replacement surgery. New minimally invasive approaches appear to decrease the recovery time from this operation.
Lethality
Osteoarthritis of the knee is not deadly.
Pain
Osteoarthritis of the knee indeed can and usually does cause pain. Other symptoms include swelling stiffness sometimes warmth and joint deformity.
Debilitation
Osteoarthritis of the knee is progressive and when it becomes severe it indeed can severely affect one’s ability to walk climb stairs enter or exit a vehicle and enjoy one’s day-to-day activities.
Comfort
Osteoarthritis of the knee indeed can and usually does cause pain and discomfort. Other symptoms include swelling stiffness sometimes warmth and joint deformity.
Curability
Osteoarthritis of the knee is not curable. However while it is not “curable ” it most certainly is treatable using activity modifications medications injections and if those interventions don’t work knee replacement surgery. New minimally invasive approaches appear to decrease the recovery time from this operation.
Fertility and pregnancy
Osteoarthritis of the knee will not affect a patient’s ability to get pregnant or have children. However some medications used to treat arthritis need to be used with care (or not at all) during a pregnancy. It is important to inform one’s obstetrician and family physician about all medications and nutritional supplements that one takes.
Independence
Osteoarthritis of the knee indeed can affect one’s ability to walk climb stairs enter or exit a vehicle and enjoy one’s day-to-day activities. These things do affect one’s ability to remain independent particularly as the disease reaches its more severe stages.
Mobility
When osteoarthritis of the knee becomes severe it indeed can severely affect one’s ability to walk climb stairs enter or exit a vehicle.
Daily activities
Osteoarthritis of the knee can affect one’s ability to walk climb stairs enter or exit a vehicle perform housework and enjoy one’s day-to-day activities. Even mild to moderate osteoarthritis of the knee can adversely impact athletic performance and enjoyment of sports particularly impact sports and sports that involve running. Although there is little “hard science” on this point most knee surgeons and rheumatologists (doctors who treat arthritic conditions non-operatively) believe that patients with osteoarthritis of the knee should consider avoiding impact sports such as running in order to avoid increasing the rate at which the disease progresses.
Energy
Many patients indeed find that the chronic pain associated with osteoarthritis of the knee does contribute to fatigue. Osteoarthritis of the knee does not affect metabolism but some patients attribute weight gain to the inactivity that results from the knee pain caused by osteoarthritis of the knee.
It is important that patients with osteoarthritis of the knee avoid decreasing their activity level and it is important that they remain fit. However this often does require some modification of exercise programs – running and walking programs are usually poorly tolerated by (and not recommended for) patients with osteoarthritis of the knee. Stationary bike swimming and water aerobics usually are well-tolerated and they are recommended.
Diet
Diets do not cure or treat osteoarthritis so far as we know. However it is important to try to avoid weight gain when one has osteoarthritis of the knee as increased body weight is associated with worsening of symptoms.
Relationships
Osteoarthritis of the knee can affect relationships and social interactions to the extent that it makes getting around more difficult.
Other impacts
Osteoarthritis of the knee is not contagious and doesn’t predispose one to other diseases or conditions. Osteoarthritis of the knee is associated with joint deformity (such as bowing of the legs “knock-knees” and loss of the ability to fully straighten or fully bend the affected knee; See Fig 5). These joint deformities are not readily managed by interventions other than surgery but can be corrected at the time of knee replacement for patients who elect to have that surgery. New minimally invasive approaches appear to decrease the recovery time from this operation.
Incidence
It is not possible to predict who will get osteoarthritis of the knee. However there are some risk factors that may increase the likelihood that knees will become arthritic. These risk factors include:
- Genetics. Arthritis often runs in families.
- Severe trauma. Fractures (broken bones) and total removal of the supporting cartilages of the knee (meniscus) both increase the likelihood of knee arthritis.
- Obesity. This is associated with arthritis of the knees.
Acquisition
Osteoarthritis is not caused by an infection though severe bacterial infections certainly can cause “post-infectious arthritis ” which is in many ways even worse than osteoarthritis of the knee.
There are some risk factors that may increase the likelihood that knees will become arthritic. These risk factors include:
- Genetics. Arthritis often runs in families.
- Severe trauma. Fractures (broken bones) and total removal of the supporting cartilages of the knee (meniscus) both increase the likelihood of knee arthritis.
- Obesity. This is associated with arthritis of the knees.
Genetics
Some arthritis indeed appears to run in families.
Communicability
Osteoarthritis of the knee is not contagious.
Lifestyle risk factors
There are two important “environmental” risk factors associated with arthritis of the knee. These are:
- Severe trauma. Fractures (broken bones) and total removal of the supporting cartilages of the knee (meniscus) both increase the likelihood of knee arthritis.
- Obesity. This is associated with arthritis of the knees.
Injury & trauma risk factors
Severe trauma including fractures (broken bones) that involve the knee joint can in time result in arthritis of the knee. Whether this really is “osteoarthritis” or should be considered a separate kind of arthritis (post-traumatic arthritis) remains an open question though in the severe stages of this condition the treatments are the same. In the ‘60s and ‘70s it was common for surgeons to remove the supporting cartilages of the knee (meniscus) if the meniscus was torn as part of a trauma. It is now known that this too results in the development of knee arthritis. As a result of learning this fact surgeons now either try to repair or minimize the portion of the meniscus that is removed should it become torn.
Prevention
By maintaining an ideal body weight and avoiding severe trauma to the knee it is possible to minimize the risk of arthritis. However many patients with osteoarthritis are slender and have never severely injured their knees so there is no “guaranteed” way to avoid getting this condition.
Anatomy
Osteoarthritis of the knee occurs when the joint surface cartilage (also called hyaline cartilage or articular cartilage) becomes worn away leaving the raw bone beneath exposed. The cartilage normally serves as a “pad” or a bearing in the joint and under normal conditions the cartilage bearing is even slicker than a hockey puck on ice. When the bearing wears away the result is a roughed joint surface that causes the pain and stiffness that people associate with osteoarthritis.
Initial symptoms
Pain swelling and stiffness are the main symptoms of knee arthritis. When it becomes more advanced joint deformity (knock-knees or bow-legs) can occur.
Symptoms
Pain stiffness swelling and joint deformity are the symptoms of arthritis of the knee.
Progression
Early in the course of arthritis the symptoms can be intermittent perhaps related only to particular activities or sustained activity. At that point usually rest and avoiding the precipitating activity will improve the symptoms. As the arthritis worsens the symptoms can become more persistent or more severe such that simply walking on level ground can result in pain.
When arthritis is severe the pain with activities can linger even after the activity stops such that the knee can remain painful even after one stops walking.
Conditions with similar symptoms
Other forms of arthritis can cause similar symptoms to osteoarthritis of the knee; in particular post-traumatic arthritis and post-meniscectomy arthritis are almost indistinguishable in many cases from osteoarthritis of the knee. Rheumatoid arthritis the next most common cause of arthritis can also affect the knee. It tends to cause other joints to be involved and often causes more of an inflammatory set of symptoms (swelling and warmth as well as pain) and can in fact effect other organ systems as well. The diagnosis of osteoarthritis versus rheumatoid arthritis can be made by a physician with experience in treating conditions of this type.
Causes
No one knows what causes osteoarthritis of the knee. However there are some risk factors that may increase the likelihood that knees will become arthritic. These risk factors include:
- Genetics. Arthritis often runs in families.
- Severe trauma. Fractures (broken bones) and total removal of the supporting cartilages of the knee (meniscus) both increase the likelihood of knee arthritis.
- Obesity. This is associated with arthritis of the knees.
Effects
Pain swelling and stiffness are the main symptoms of knee arthritis. When it becomes more advanced joint deformity (knock-knees or bow-legs) can occur. As the condition worsens it often becomes less responsive to medical treatments such as pills or injections.
In many patients with advanced arthritis particularly if those medical approaches are no longer helpful surgery can offer relief of symptoms. Some patients with severe osteoarthritis sometimes can benefit from joint replacement surgery either partial (unicompartmental) knee replacement or total knee replacement which now can be done using a minimally-invasive quadriceps-sparing approach that can significantly shorten the recovery and decrease the pain following surgery.
Diagnosis
To diagnose osteoarthritis of the knee a physician will take a thorough history and perform a thorough physical examination first. Following this simple x-rays taken with the patient standing are an effective way to diagnose this condition.
Diagnostic tests
The simplest test to diagnose osteoarthritis of the knee is the x-ray. Taken with the patient standing up plain x-rays can diagnose the condition with great accuracy.
Very mild arthritis can be seen on a bone scan or an MRI even before it is visible on plain x-rays but in reality these tests are seldom helpful clinically for this purpose.
Effects
The diagnostic tests for osteoarthritis of the knee including x-rays and MRIs are generally not painful and they are well-tolerated by most patients.
Health care team
Osteoarthritis of the knee is common and generally straightforward to diagnose. Family physicians internists orthopedic surgeons rheumatologists and physiatrists often are the ones who make the diagnosis of osteoarthritis of the knee.
Finding a doctor
Both rheumatologists and orthopedic surgeons are “specialists” in arthritis care.
If surgery is being considered to manage osteoarthritis of the knee visiting with a fellowship-trained high-volume knee replacement surgeon would be a reasonable step to consider.
Treatment
Simple steps that can be taken which don’t have much risk include avoidance of the activities that cause symptoms (activity modification) and weight loss (if appropriate). Some patients find nutritional supplements such as glucosamine and chondroitin to be helpful; however the data on these products is somewhat inconsistent. They don’t help everyone.
Some patterns of osteoarthritis of the knee can be treated with an arthritis brace such as a knee sleeve or an “Unloader” type brace.
Should those interventions not be satisfying in consultation with one’s physician the next steps might include over-the-counter pain remedies such as acetaminophen (Tylenol) and over-the-counter anti-inflammatories such as ibuprofen (Advil Motrin) or naproxen (Naprosyn) among others. However these pills are not for everyone and if one hasn’t used them before one should consider consulting one’s family physician first. Sometimes prescription-strength non-steroidal anti-inflammatory drugs (NSAIDs) can be prescribed but again this must be done in consultation with a physician and these drugs do have risks and side effects associated with them.
In general narcotic pills (“painkillers” like Tylenol #3 Vicoden Percocet oxycodone) and narcotic pain patches (fentanyl Duragesic) should be avoided for most patients with osteoarthritis of the knee.
Joint injections including intra-articular corticosteroid injections and “viscosupplement” injections like Synvisc Hyalgan Supartz and others can be helpful for some patients.
Patients with severe arthritis who have tried the above remedies sometimes can benefit from joint replacement surgery either partial (unicompartmental) knee replacement or total knee replacement which now can be done using a minimally-invasive quadriceps-sparing approach that can significantly shorten the recovery and decrease the pain following surgery.
Not all surgical cases are the same, this is only an example to be used for patient education.
Self-management
Keeping one’s body weight appropriate and choosing activities that don’t reproduce the arthritic pain are two things patients with osteoarthritis of the knee can do to help decrease the arthritic symptoms.
Health care team
Several kinds of health care providers participate in the management of osteoarthritis of the knee including:
- Family physicians and internists
- Rheumatologists
- Physical Medicine and Rehabilitation Specialists (Physiatrists)
- Orthopedic Surgeons
Pain and fatigue
Several approaches can be used to manage the pain associated with osteoarthritis of the knee including:
- Activity modification appropriate kinds of exercise and weight loss when necessary may alleviate some knee arthritis symptoms
- Nutritional supplementation (glucosamine and chondroitin) are helpful to some patients although the literature on these supplements is not consistently in favor of their use
- Non-narcotic pain tablets (acetaminophen/Tylenol) or over-the-counter non-steroidal anti-inflammatory drugs if medically appropriate sometimes are helpful
- Prescription strength non-steroidal anti-inflammatory drugs (NSAID) are useful for some patients though in general long-term use of these drugs is discouraged
- Arthritis unloader braces or knee sleeves are helpful for some patterns of arthritis
- Joint injections (corticosteroid or “cortisone” injections; or “viscosupplement” injections such as Hyalgan Synvisc Orthovisc or Supartz) might help
- Total knee replacement surgery may be used if non-operative interventions don’t suffice; a minimally-invasive quadriceps-sparing approach can decrease the post-operative pain and length of convalescence in some patients undergoing this procedure.
Diet
Keeping one’s weight proportional to one’s height can decrease the likelihood of developing osteoarthritis of the knee and can decrease the symptoms of the condition once it has set in.
Exercise and therapy
There is some evidence that appropriately-designed exercise programs can decrease the pain of knee arthritis in particular earlier stages of the condition. Gentle strengthening of the quadriceps (front of the thigh) muscles such as by using a stationary bicycle is probably the most effective approach for this.
Medications
- Nutritional supplementation (glucosamine and chondroitin) are helpful to some patients although the literature on these supplements is not consistently in favor of their use
- Non-narcotic pain tablets (acetaminophen/Tylenol) or over-the-counter non-steroidal anti-inflammatory drugs if medically appropriate sometimes are helpful
- Prescription strength non-steroidal anti-inflammatory drugs (NSAID) are useful for some patients though in general long-term use of these drugs is discouraged
- Joint injections (corticosteroid or “cortisone” injections; or “viscosupplement” injections such as Hyalgan Synvisc Orthovisc or Supartz) might help
Narcotic painkillers whether in pill form (oxycodone Tylenol #3 Vicoden Percocet Lortab etc. or patch form (Duragesic fentanyle etc.) in general should be avoided for the treatment of osteoarthritis of the knee.
Surgery
Knee replacement is a surgical procedure that decreases pain and improves the quality of life in many patients with severe arthritis of the knees. Typically patients undergo this surgery after non-operative treatments (such as activity modification anti-inflammatory medications or knee joint injections) have failed to provide relief of arthritic symptoms. Surgeons have performed knee replacements for over three decades generally with excellent results; most reports have ten-year success rates in excess of 90 percent.
Broadly speaking there are two types ways to insert a total knee replacement: the traditional approach and the newer minimally-invasive (sometimes called quadriceps-sparing) approach.
Traditional total knee replacement involves a roughly 8” incision over the knee a hospital stay of 3-5 days and sometimes an additional stay in an inpatient rehabilitation setting before going home. The recovery period(during which the patient walks with a walker or cane) typically lasting from one to three months. The large majority of patients report substantial or complete relief of their arthritic symptoms once they have recovered from a total knee replacement.
Minimally-invasive quadriceps-sparing total knee replacement is a new surgical technique that allows surgeons to insert the same time-tested reliable knee replacement implants through a shorter incision using surgical approach that avoids trauma to the quadriceps muscle (see figure 1) which is the most important muscle group around the knee. This new technique which is sometimes called quadriceps-sparing knee replacement uses an incision that is typically only 3-4” in length (see figure 2) and the recovery time is much quicker – often permitting patients to walk with a cane within a couple of weeks of surgery or even earlier. The less-traumatic nature of the surgical approach also may decrease post-operative pain and diminish the need for rehab and therapy compared to more traditional approaches.
The main potential benefits of this new technique include:
More rapid return of knee function. Patients who undergo this procedure seem to get muscle strength and control back more quickly than patients who have had traditional total knee replacement. (See Video) This is because the quadriceps muscle and tendon are not divided in the course of the surgical exposure like in traditional knee replacement and the kneecap is not everted (flipped out of the way) as it is in traditional total knee replacement.
Smaller incision. While this procedure would not be worth performing for cosmetic benefits many patients do prefer the shorter incision. Traditional knee replacement incisions often measure 8” or longer; minimally-invasive quadriceps-sparing knee replacement incisions are about 4” in length for most patients.
Decreased post-operative pain. (See Video)This may be a function of the smaller incision and the fact that the incision stays out of the important quadriceps muscle/tendon group.
Same reliable surgical implants as Traditional Knee Replacement. Much has been learned about implant design in the nearly 40-year history of contemporary knee replacement. Minimally-invasive quadriceps-sparing total knee replacement is an evolution of surgical technique which permits the use of time-tested implant designs (see figure 3 and figure 4). This gives some reassurance that while the surgical approach is new the implants themselves have a good proven track record.
The major apparent risks of the procedure compared to traditional total knee replacement:
The procedure is new. Though surgeons have studied the approach the studies are recent and have replicated (repeated and verified) by only a few groups of surgeon-scientists. These studies give some insight into which patients and patterns of arthritis are most suitable for this procedure the relative novelty of the approach it is likely that as time passes we will discover more about the risks and shortcomings of this technique. Also even an experienced knee replacement surgeon will have performed many more surgeries through the traditional approach than through the less-invasive method; we know that the more procedures one does the more reliable the results are.
The procedure is more challenging. Operating through a smaller surgical window takes some getting used to and this can increase operative time compared to procedures performed using the traditional technique. This may increase the likelihood that an intra-operative injury to tendon or ligament might occur which could compromise the result. This may also increase the likelihood of component malalignments which could affect function and durability. However two preliminary studies on this technique in fact found that these adverse outcomes did not take place.
Joint aspiration
Joint injections can be effective at relieving the symptoms associated with osteoarthritis of the knee. Broadly speaking there are two kinds of injections:
- Corticosteroid injections (“cortisone shots”).These injections have been used to relieve arthritis symptoms--including pain swelling and inflammation--for over 50 years. Despite this there have been surprisingly few well-designed scientific studies to determine which patients might benefit from this treatment or how long the relief might last. Just the same cortisone shots are commonly used--and often are successful--in helping to relieve arthritis symptoms temporarily. Some patients are able to use them to get enough pain relief to hold off joint replacement surgery for months or even years. Cortisone shots are a treatment for pain; they do not alter the course of arthritis and they do not cure the condition.
- “Viscosupplement” injections. These are any of several compounds that are made up of hyaluronic acid which is a component of normal joint fluid. Some of the common ones include Synvisc Hyalgan Supartz and Orthovisc. They are given as a series of injections usually weekly for 3-5 weeks. There is some disagreement as to how and whether they work. Read more details on JBJS Article - Corticosteroids VS. Hylan GF20 in pdf format (0.13MB).
Splints or braces
Two kinds of braces are sometimes used:
- Over-the-counter knee sleeves usually made of neoprene (wet suit material). These can be purchased at drug stores and medical supply houses and some patients find them to be supportive and comfortable.
- Arthritis “Unloader” braces. These are custom-fitted to the knee by a bracing specialist (an orthotist) and a prescription is needed. They are not for every pattern of arthritis and work best if the arthritis is limited either to the inside or the outside of the knee. They can be expensive; insurance sometimes covers part or all of the cost.
Alternative remedies
Nutritional supplementation (glucosamine and chondroitin are the most common forms of this) is helpful to some patients though the science on this is not entirely supportive of their effectiveness.
There are some studies to suggest that acupuncture can decrease the pain associated with osteoarthritis of the knee.
Work
Looking for a “light duty” alternative to heavy manual labor is one good approach for coping with osteoarthritis of the knee. Many patients who work at desks find that prolonged sitting in one position is associated with stiffness and pain upon first arising so periodically standing stretching or moving the knee through an arc of motion can be helpful at minimizing this “start-up” pain.
Adaptive aids
For some patients particularly those who cannot tolerate surgical interventions for medical or other personal reasons use of a cane crutches or a walker can be of use.
Resources
For more information about arthritis contact the Arthritis Foundation (www.arthritis.org). For more information about orthopedic surgery contact the American Academy of Orthopedic Surgeons (www.aaos.org).
Condition research
Medical researchers continue to look into the causes and best treatments for symptoms of osteoarthritis of the knee which is very common and sometimes disabling.
Pharmaceutical research
There is considerable research being done into the medical management of osteoarthritis. Recently increasing awareness of the complications and problems associated with use of non-steroidal anti-inflammatory drugs (NSAIDs) including effects on the kidneys the stomach and the heart.
Surgical research
There is considerable research being done studying the surgical approaches for this condition including newer approaches for total knee replacements; one of these the minimally-invasive quadriceps sparing approach appears to help patients recover more quickly and with less pain than traditional approaches to knee replacements.
Other surgical interventions including osteotomy (cutting and re-orienting the bones around the knee) and arthroscopy (using a surgical camera and small motorized shavers to “clean up” the raw bone ends) also are topics of surgical research relevant to patients with knee arthritis.
Summary of knee arthritis
- Osteoarthritis of the knee is common and can result in severe pain and disability; as a result of this condition several hundred thousand people each year in the U.S. undergo total knee replacement.
- Most people with osteoarthritis of the knee can be managed without surgery.
- The cause of osteoarthritis of the knee is not known but some risk factors include obesity severe knee trauma and genetics.
- There are many other kinds of arthritis that can affect the knee; it is important to make sure that the correct diagnosis is made as some of these other conditions are treated very differently.
- The diagnosis of osteoarthritis of the knee is usually very straightforward and is made in almost all cases by a physician taking a thorough history performing a physical examination and getting x-rays with the patient standing up.