Last updated: January 28, 2013
Overview
Total hip resurfacing arthroplasty is a bone-preserving procedure that helps restore comfort and function to patients’ hips damaged by degenerative joint disease (osteoarthritis rheumatoid arthritis and traumatic arthritis) avascular necrosis or developmental hip dysplasia. It is viewed as an alternative to traditional hip replacements for helping patients return to their active lifestyles.
There has been a recent surge in interest in hip-resurfacing procedures. Advocates have pointed to the bone-conserving nature of the procedure and anticipated potential benefits related to post-operative activities and range of motion. IMAGE 1 illustrates the difference in the amount of bone removed for a resurfacing procedure versus a traditional total hip replacement procedure. In this procedure surgeons replace the acetabulum (hip socket) in much the same way as a conventional total hip replacement but the femoral head is resurfaced rather than removed.
Video
Bone Sparing Total Hip Resurfacing Arthroplasty Surgery
Hip resurfacing is intended for patients with high functional demands for whom traditional total hip arthroplasty would be a poor option because of anticipated failure in the future and subsequent revision surgery.
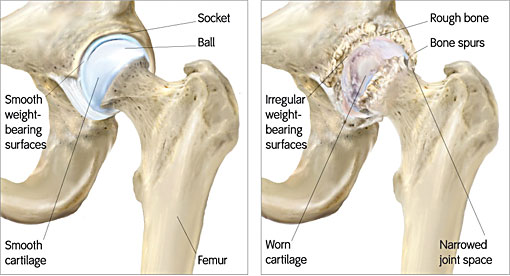
In these patients the hip-joint surface – the socket side on the pelvis and the top end of the femur which fits into the socket – is destroyed by wear and tear inflammation or prior injury (IMAGE 2). This leads to stiffness pain and decreased ability to perform at work or enjoy leisure activities such as sports.


The goal of hip resurfacing is to restore the best possible function to the joint by replacing damaged joint surfaces with artificial ones. After a clinical exam an orthopedic surgeon with training in hip-resurfacing can help a patient determine if this procedure would be helpful.
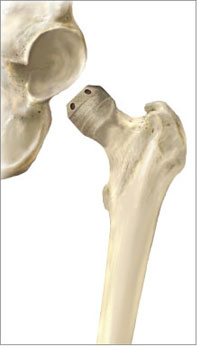
Modern hip-resurfacing systems involve placing a non-cemented porous metal cup into the hip socket and cementing a metal cap onto the femoral head. This results in an articulating metal-on-metal surface (IMAGE 3).
Only as recently as May 2006 did the FDA approve the first U.S.-available device for the procedure manufactured by Smith & Nephew. Its device has been implanted in about 80 000 hips worldwide since 1997. A similar device made by Corin Group was approved for U.S. use in July 2007 and other manufacturers sell such devices around the world.
Total hip resurfacing arthroplasty is a technical procedure best performed by a surgical team trained in this surgery. Such a team can maximize the benefit and minimize risks. The procedure is performed under general or spinal anesthesia.
Many individuals are not appropriate candidates for total hip resurfacing arthroplasty. For example patients with poor bone stock significant avascular necrosis of the femoral head kidney dysfunction infection leg-length discrepancy or women of child-bearing age may not be suitable patients for this procedure. A thorough discussion with your orthopedic surgeon is necessary to determine whether this procedure is an option.
Not all surgical cases are the same, this is only an example to be used for patient education.
Possible benefits of total hip resurfacing arthroplasty
Hip resurfacing may lead to a dramatic improvement in the quality of life of young active patients who have advanced arthritis of the hip. When combined with a thoughtful rehabilitation program total hip resurfacing arthroplasty allows patients with arthritic hips to regain comfort and function. The procedure has been shown in intermediate term studies (10 years of follow-up) to have met patient expectations with an extremely low failure rate. Many patients have returned to pre-symptomatic levels of activities (sports cycling etc.) and occupation several months after this procedure.
Hip resurfacing can improve the mechanics of the hip but cannot make the joint as good as it was before the onset of arthritis. In many cases the muscles and tissues around the hip have been weakened from prolonged disuse before the hip-resurfacing procedure. After surgery it usually takes time for a patient to realize maximal improvement.


Who should consider total hip resurfacing arthroplasty?
Young active patients should consider hip resurfacing when:
- arthritis has been resistant to conservative measures;
- the patient is sufficiently healthy to undergo the procedure;
- the patient understands the risks and alternatives;
- the surgeon is trained and experienced in hip-resurfacing surgery;
- no medical or surgical contraindication to hip resurfacing exists.
What happens without surgery?
Pain can be managed with medicine assistive devices and some alternative therapies. For some young active patients nonsurgical management of debilitating advanced hip arthritis is not satisfactory.
Effectiveness
In the hands of an experienced surgeon trained in hip resurfacing total hip resurfacing arthroplasty is effective in restoring comfort and function to the hip of a well-motivated patient. A 2007 study of 59 hips reported significant improvement in pain function range of motion and activity among patients who were on average six years postoperative. The study published in The Journal of Bone and Joint Surgery by H.C. Amstutz and colleagues at the Joint Replacement Institute reported five cases (8 percent) of femoral failure requiring subsequent total hip arthroplasty.
This and other studies have helped physicians better discern which patients have a better chance of a successful outcome.
Although hip resurfacing can allow a patient to resume some physical activities high-impact activities such as running basketball and singles tennis are more likely to lead to earlier loosening of the implant and need for revision surgery.
Urgency
Total hip resurfacing arthroplasty is not considered urgent. It is an elective procedure that can be scheduled when circumstances are optimal. The patient has time to become informed and to select an experienced surgeon. Before surgery is undertaken the patient should:
- be in optimal health;
- understand and accept the risks and alternatives of surgery;
- understand and be committed to the postoperative rehabilitation program.
Risks
The most common risk of hip resurfacing is fracture of the femoral neck. In one study the rate of fracture was 1.46 percent. The procedure’s technical challenges and patient selection might increase risk of fracture. Infection is a rare but potentially catastrophic risk. Component loosening is an infrequent complication according to published literature.
Potential risks exist from the production of metal ions (cobalt and chromium) caused by the rubbing of the metal implant’s components. Proper component positioning appears to be essential to reducing significant production of metal ions. There is a theoretical concern that these ions may pose a cancerous risk – though long-term data does not currently support this assertion. But a patient who has kidney problems might have difficulty filtering these ions from the blood; he or she should avoid implantation of metal-based hip components.
For the same reason hip resurfacing also is not recommended for women of childbearing age who plan to have children because of the uncertainty about the effects of metal ions on the developing fetus.
Hypersensitivity to metal ions is a risk that is being increasingly recognized and may lead to loosening of the components. While little correlation appears to exist between skin hypersensitivity and metal hypersensitivity in the hip joint hip resurfacing is not recommended for people with documented allergies to metal or jewelry.
A thorough preoperative evaluation in preparation for surgery is important for minimizing potential risks of hip resurfacing surgery. For example some patients will need a formal cardiology evaluation in addition to a general orthopedic evaluation if there is a significant history of heart disease. An experienced joint replacement team will use special techniques to minimize the risk of many of the above mentioned complications but cannot always totally eliminate them.
Managing risk
Many of the risks of total hip resurfacing arthroplasty can be effectively managed if they are promptly identified and treated. A coordinated effort at managing risks should be undertaken by the orthopedic surgeon in conjunction with the patient’s primary care doctor. Infection might require a washout in the operating room or an exchange of components. Loosening of the components might require revision surgery. Fracture usually requires revision to a conventional total hip arthroplasty. This can be accomplished relatively easily by removing the femoral resurfacing cap and implanting a standard long-stemmed femoral head and neck device as with total hip replacement. The patient should contact the surgeon with any questions or concerns about risks.
Preparation
Total hip resurfacing arthroplasty is an option for healthy active and motivated individuals in whom arthritis interferes with hip function.
A successful outcome can be influenced by good communication between the patient and the surgeon. Patients should optimize their health prior to surgery. Smoking should be stopped a month before surgery and not resumed for at least several months afterwards (if ever). Any heart lung kidney bladder or dental problems should be managed before surgery; infection could be a reason to postpone surgery. The hip surgeon needs to be aware of all health issues including allergies and the non-prescription (herbal medicines St. John’s wort etc.) and prescription medications being taken. Some of these medicines might need to be discontinued before surgery – especially those that may increase a patient's likelihood to bleed. Since blood transfusion might be necessary patients may choose to have a blood bank draw and store their own blood for a possible transfusion.
Before surgery patients should consider the limitations alternatives and risks of surgery. Patients should also recognize that the result of surgery depends in large part on their efforts in rehabilitation after surgery.
It is recommended that patients continue to walk and exercise if possible before surgery so that the muscles around the hip are not overly deconditioned.
The patient must plan to be less functional than normal immediately after surgery. Driving shopping and performing usual work or chores likely will be difficult during this time. Plans for necessary assistance should be made before surgery. For individuals who live alone or those without readily available help arrangements for home help should be made well in advance.
Timing
Total hip resurfacing arthroplasty can be delayed until the time that is best for the patient’s overall well-being.
Costs
The patient’s insurance provider can provide a reasonable estimate of the following:
- the surgeon's fee
- the hospital fee
- the degree to which these should be covered by the patient's insurance
Surgical team
Total hip resurfacing arthroplasty is a technically demanding procedure that should be performed by an experienced surgeon in a medical center accustomed to performing hip replacements at least several times a month.
Finding an experienced surgeon
Because the resurfacing-arthroplasty devices have received approval only recently in the United States many communities do not have surgeons trained in this procedure. The device manufacturers require that surgeons who implant their devices be properly trained for technique. Surgeons specializing in hip joint replacement may be located through the American Academy of Orthopedic Surgeons Web site university schools of medicine county or state medical or orthopedic organizations.
Facilities
Total hip resurfacing arthroplasty is usually performed in a major medical center whose surgeons perform these procedures on a regular basis. These centers have surgical teams and facilities specially designed for such surgery. They also have nurses and therapists accustomed to assisting patients in their recovery from hip-replacement surgery.
Technical details
After the anesthetic has been administered and the hip is prepared the surgeon makes an incision. Most surgeons approach the joint from the posterior (rear); others prefer a lateral (side) or anterior (front) approach. During the posterior approach fibers of the gluteus maximus muscle are split. The tendinous insertion of the gluteus maximus is recessed or divided to allow movement of the femur bone.
The interval between the gluteus minimus and the superior acetabulum (hip socket) is developed and the piriformis tendon is released from its femoral attachment. A 360-degree capsulotomy is then performed.
The acetabulum is prepared. Bone spurs are removed. Reamers are used to enlarge the acetabulum in preparation for placement of the cup whose position is crucial for a successful outcome. The cup is impacted into place.
The femur is prepared by using an alignment guide. A guide wire ensures that the spherical metal cap is positioned correctly on the femoral head. The surgeon with a chamfering router-like instrument removes only the outer layer of the femoral head so that the cap will fit snugly (IMAGE 4). After the femur has been prepared cement is mixed and the femoral cap component is impacted into place also secured by a metal stem that extends into the femoral neck. (The femoral neck is left intact.)
With the femur and acetabulum completed the hip joint is re-established (IMAGE 5) and taken through a range of motion to test stability. The soft tissues are repaired and the remainder tissues are closed in layers and a dressing applied to the wound.
Anesthetic
Hip-resurfacing surgery can be performed under a general anesthetic or under a regional block (epidural or spinal). A spinal block can provide anesthesia for several hours after the surgery. The patient may wish to discuss their preferences with the anesthesiologist before surgery.

Length of total hip resurfacing arthroplasty
The procedure usually takes about two hours however the preoperative preparation and postoperative recovery may add several hours of time. Patients often spend two hours in the recovery room and on average three days in the hospital after surgery.
Pain and pain management
Hip-resurfacing surgery is a major surgical procedure that involves cutting of skin preparation of bone as well as suturing of tendons. The pain from this surgery is managed by the anesthetic and by pain medications. Immediately after surgery strong medications (such as morphine or Demerol) may be given by injection. Within a day or so oral pain medications – strong painkillers and non-narcotic painkillers such as Tylenol (acetaminophen) – are usually sufficient.
Use of medications
Initially pain medication usually is administered intravenously or intramuscularly – and sometimes patients are allowed to administer the medication as they need. Hydrocodone or Tylenol with codeine are taken by mouth. Intravenous pain medications are usually needed only for the first day or two after the procedure. Oral pain medications are usually needed only for the first two weeks after the procedure.
Effectiveness of medications
Pain medications can be very powerful and effective. Their proper use lies in balancing their pain-relieving effect and their other less desirable effects. Good pain control is an important part of the postoperative management.
Important side effects
Pain medications can cause drowsiness slowed breathing difficulties in emptying the bladder and bowel nausea vomiting and allergic reactions. Patients who have taken substantial narcotic medications in the recent past may find that usual doses of pain medication are less effective. For some patients balancing the benefit and the side effects of pain medication is challenging. Patients should notify their surgeon if they have had previous difficulties with pain medication or pain control.
Hospital stay
After surgery the patient spends an hour or so in the recovery room. A drainage tube may be used to remove excess fluid from the surgical area. Such a drain would be removed on the first or second day after surgery. Bandages cover the incision. They are usually changed the second day after surgery.
Patients are discharged as soon as the incision is dry the hip’s pain is manageable with oral pain medications the patient can perform the range-of-motion exercises and support systems are in place at the patient’s home. Discharge is usually on the third day after surgery.
Recovery and rehabilitation in the hospital
Early mobilization after total hip resurfacing arthroplasty helps achieve the best possible hip function. Arthritic hips are stiff and one major goal of hip resurfacing is to relieve much of this stiffness. However after surgery scar tissue will tend to recur and limit movement unless mobilization is started immediately. This early mobilization is facilitated by the complete surgical release of the tight tissues.
The night of surgery patients are encouraged to get up to use a commode or walk to the bathroom with assistance.
During the hospitalization the patient learns a simple rehabilitation program that will help maintain mobility at home after discharge. On the day of surgery or the day after the physical therapist teaches the patient gentle exercises. The patient usually is shown how to prevent stiffness and adhesions.
Walking and strengthening exercises are encouraged soon after surgery. Many patients return to leisure activities within 3-6 months after surgery.
Hospital discharge
At the time of discharge the patient should be relatively comfortable on oral medications should have a dry incision should understand their exercises and should feel comfortable with the plans for walking. For the first month or so after this procedure the operated leg may be less useful than it was immediately beforehand.
Limitations can be specified only by the surgeon who performed the procedure. It is important that the repaired tissues not be challenged until they have had a chance to heal.
The patient must plan to manage the activities of daily living during the period of recovery.
Convalescent assistance
Patients usually require assistance with self-care activities of daily living shopping and driving for four to six weeks after surgery. In the absence of home support a convalescent facility may provide a safe environment for recovery.
Recovery of comfort and function after hip resurfacing continues for many months after the surgery. Improvement in some activities may be evident as early as two weeks. With persistent effort patients make progress for as long as three to six months after surgery.
Physical therapy
Early mobilization after hip resurfacing is critical for achieving optimal function.
Arthritic hips are stiff. One of the major goals of total hip resurfacing arthroplasty surgery is to relieve much of this stiffness. However after surgery scar tissue will tend to emerge and will limit movement unless mobilization is started immediately. This early mobilization is facilitated by the complete surgical release of the tight tissues so that after surgery the patient has only to maintain the motion achieved at the operation. Later on after the hip is comfortable and more flexible strengthening exercises and additional activities are started.
Rehabilitation options
It is often most effective for the patient to carry out his or her own exercises so that they are done frequently effectively and comfortably. Usually a physical therapist or the surgeon instructs the patient in the exercise program and advances it at a rate that is comfortable and beneficial for the patient. For the first six weeks after surgery emphasis is placed on optimizing mobility and strengthening. At six weeks the strengthening exercises may be gradually increased in intensity.
Can rehabilitation be done at home?
In general the exercises are best performed by the patient at home. Occasional visits to the surgeon or therapist may be useful to check the progress and to review the program.
Usual response
Patients often experience significant increases in range of motion comfort and function with this procedure and those benefits could be aided by rehabilitation. If the exercises are uncomfortable difficult or painful the patient should contact the therapist or surgeon promptly.
Risks
This is a safe rehabilitation program with little risk.
Duration of rehabilitation
Once the range of motion and strength goals are achieved the exercise program can be cut back to a minimal level. However gentle stretching is recommended on an ongoing basis.
Returning to ordinary daily activities
In general patients are able to perform gentle activities with the operated leg the day after surgery. Walking with assistance is strongly encouraged. Driving should wait until the patient can perform the necessary functions comfortably and confidently.
With the surgeon’s consent patients can often return to activities such as swimming light hiking bicycling golf and doubles tennis in three to six months after surgery.
Stressful activities and activities with the leg in extreme positions must be avoided until several months after the surgery and then only if the hip is comfortable and strong.
Long-term patient limitations
Many surgeons allow patients to return to pre-surgery activities (bicycling hiking) and an active lifestyle. While hip resurfacing implants may be more durable in the long run than traditional total hip replacement implants there are still several restrictions that should be observed. For example high impact loading (contact sports jogging etc.) on the operated hip is not recommended. If there are questions about certain activities they should be discussed directly with the surgeon.
Costs
The therapist and the patient’s insurance provider should have the information on the usual cost of the rehabilitation program.
Summary of total hip resurfacing arthroplasty for total hip resurfacing arthroplasty
Total hip resurfacing arthroplasty helps restore comfort and function to hip joints damaged by arthritis or other degenerative disorders.
Hip resurfacing is a bone-preserving procedure that is an alternative to traditional total hip replacement. However resurfacing procedure is actually more invasive than a total hip replacement surgery requiring a larger incision and a greater disturbance of soft tissue.
The main benefits of resurfacing are that the patient can be more active postoperatively than is the case with a traditional replacement and the patient is left with more bone should total hip replacement be necessary later in life.
Hip resurfacing is indicated for a subset of the population especially young active individuals. A discussion with your surgeon is necessary to determine if this surgery is appropriate for you.
A motivated patient and persistent rehabilitation efforts will help to assure the best possible results.